What you always wanted to know about DRY EYE DISEASE ... and never dared to ask !

Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT ]
More information about Dry Eye Disease
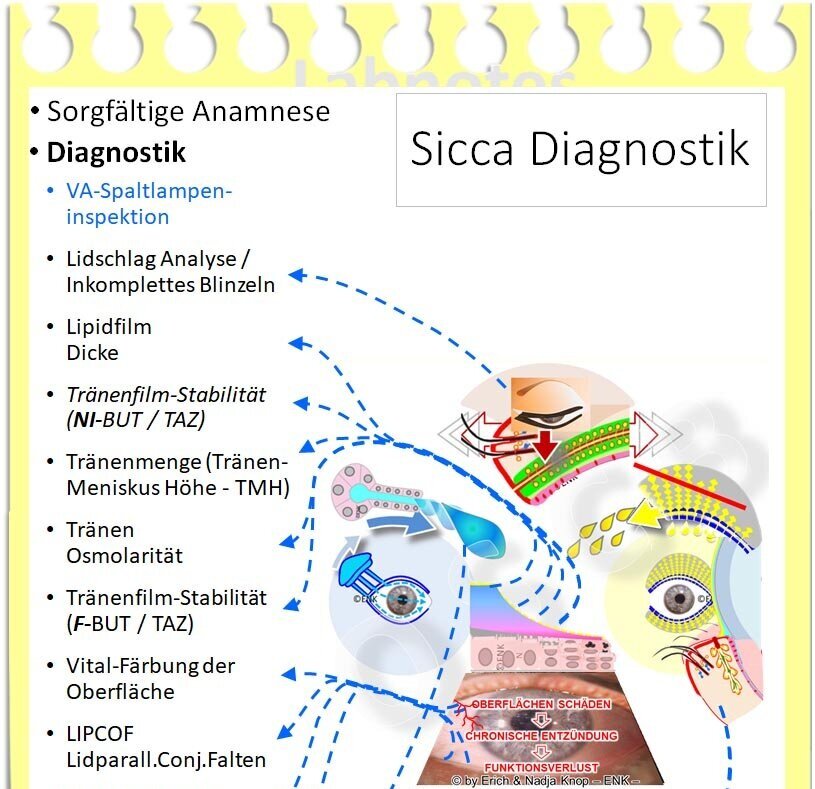
On this page you will find some more background information to better understand the preceding FACTS page
Dry eye patients have many questions
Patients with so-called 'dry eyes', typically suffer from the disease of the dry eye with the corresponding complaints. Such patients have many questions.
These questions are answered below so that patients can better understand their illness and the options for diagnosis and treatment.
Questions and answers about Dry Eye Disease
(´Click´ on an image for the answers)
1. Facts are simple
What is Dry Eye Disease ?
In medical terms it is also called Keratoconjunctivitis sicca or Sicca syndrome
The Sjogren syndrome is a very specific type of dry eyes and based on a rare disorder of the lacrimal gland
Meibomian gland dysfunction (MGD) is a common cause of dry eyes ...
... and Dry Eye Disease itself is the most common disease in ophthalmology !
2. Complaints are various
What are the symptoms and complaints of Dry Eye Disease ?
Dry eye disease can cause many different symptoms - How do I recognize a dry eye ?
My eyes are often very dry ... and I have a gritty sandy sensation like foreign bodies in my eyes !
My eyes are often burning and red ... and I always have so heavy tired eyes and eye fatigue
In the morning I often have sticky eyes and can hardly open my eyelids !
Why are my eyes often so dry ... but sometimes wet and watery ?
My vision is often blurry - but it gets better after a few eyelid blinks !
The doctor says my dry eye has gotten much better - but I'm still in a lot of pain !
What is chronic pain syndrome ?
3. Cause is a disorder of the tear film
What is the cause of Dry Eye Disease - How does dry eye disease come about ?
What is the ´ocular surface´ ?
What is the ´tear film´ ? - What is the tear film made of ?
Why are tear film disorders so harmful to the eye ?
I used to like my contact lenses - but now I can hardly tolerate them any more !
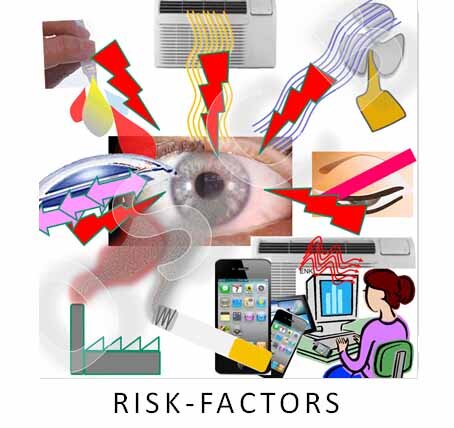
4. Risk factors are important
Are there risk factors for dry eyes ?
When I work on the computer in the office, my dry eye is worst !
I have the most complaints while driving a car !
During the heating season in winter my dry eye always gets worse !
Is it possible that chronic disease and medication can influence my dry eyes ?
after eye surgery a dry eye may occur, become worse or is first noticed
5. Dryness has various reaons
Aqueous lack of tears is usually not a primary triggering factor
… but instead, a lack of oil with subsequent evaporation of the tear water is typically much more common.
Eyelid disorders also play an important role !
The ´office eye´ combines many desiccating factors and is frequent particularly among younger people
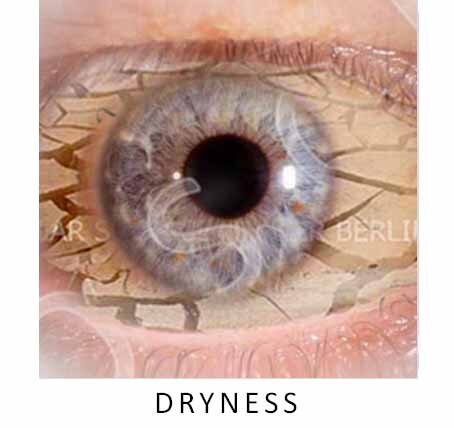
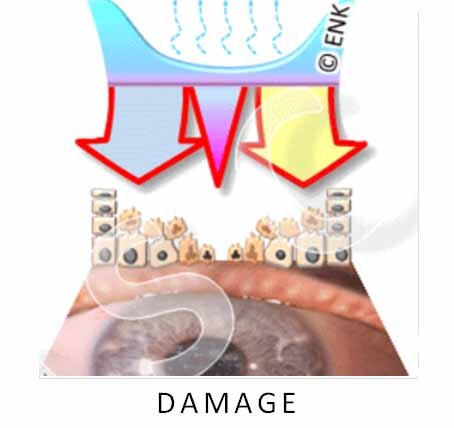
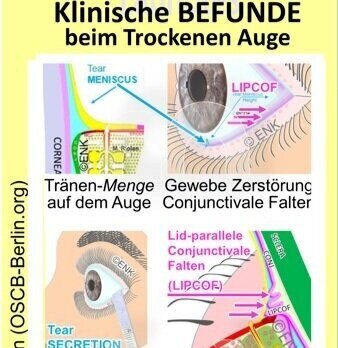
6. Damage is a consequence of dryness
Dryness leads to tissue damage
Tissue damage leads to nerve irritation with feelings of irritation and pain
Advanced Dry Eye Disease can lead to destruction of the ocular surface
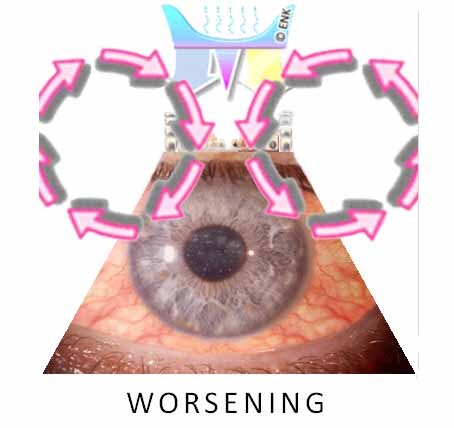
7. Worsening is typical in Dry Eyes
When does a dry eye turn into Dry Eye Disease ?
Why does Dry Eye Disease tend to get worse without adequate treatment ?
What are vicious circles of disease worsening ?
Why can a dry eye cause inflammation ?
What role does inflammation play in Dry Eye Disease ?
8. Therapy - there are several options
besides the aim to reduce risk factors as much as possible …
… there are many options for the therapy of dry eyes
What is Dry Eye Disease ?
Dry eyes, or rather the dry eye disease, is a chronic irritation and damage to the tissue at the surface of the eye.
The healthy eye surface must be moist to stay healthy - always and everywhere !!! - even with open eyelids. Therefore the ocular surface is covered by a tearfilm.
A dry eye is typically triggered by any lack or deficiency of the tear film on the eye.
This leads to eye irritation and complaints such as a gritty sandy feeling, or a burning sensation, pain, and sticky eyes.
Especially at the beginning of the condition and in people of advanced age, the irritation can also lead to wet eyes and tears running down the cheeks.
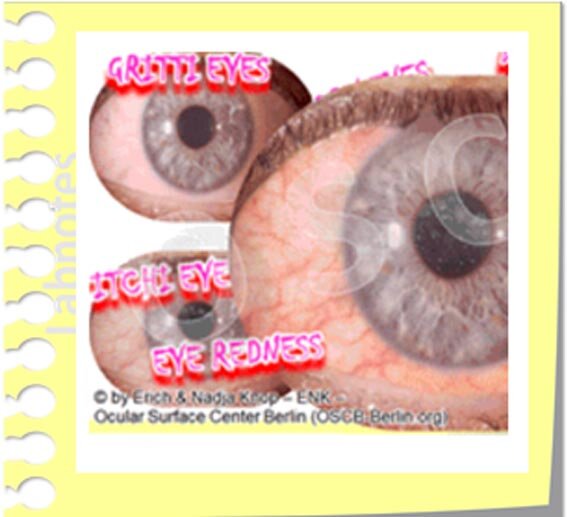
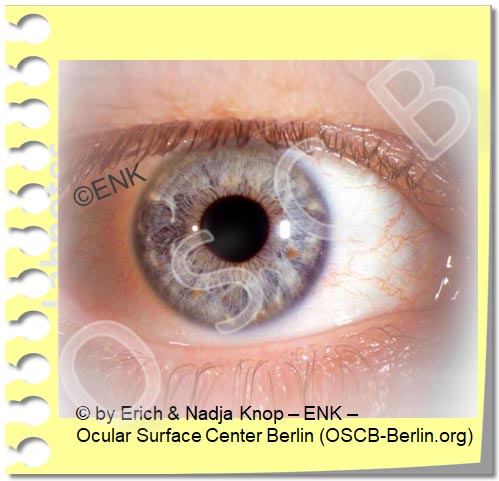
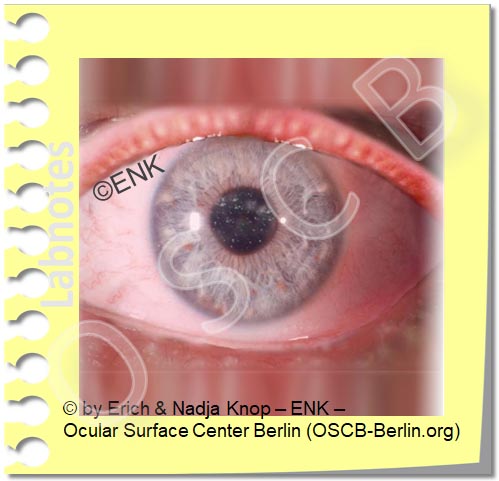
Redness
The inflammatory stimulus, which is triggered by the chronic irritation of the eye, also leads to a dilation of the blood vessels and thus to reddening of the eye.
However, the reddening is usually only moderate in this condition.
What is Keratoconjunctivitis sicca ?
The ophthalmologist also describes dry eye disease as “keratoconjunctivitis sicca” . Sicca means 'dry' and keratoconjunctivitis indicates ´inflammation´. Keratoconjunctivitis sicca therefore means " dry/ dryness inflammation of the cornea and conjunctiva ".
This term is partially misleading because many dry eye patients first have wet eyes with teardrops running over their cheeks. This is because the irritated eye tries to wash away the stimulus through strong tear production. Although it is often helpful in cases of a foreign body - this does unfortunately not help in chronic irritation of the ocular tissue itself.
In recent years it has been scientifically proven that inflammation often develops in dry eye disease. The disease and the complaints of the patient continue to worsen through the inflammatory process.
What is Sicca syndrome ?
Sicca syndrome is another medical term for dry eye disease.
Here, too, the term ´sicca´ focuses on dryness of the eye - which is not always the case as mentioned before, since many patients can have a wet eye, at least initially.
The term ´syndrome´ describes that this condition leads to a ´bundle´ of different complaints in the patient. At first glance, these various complaints may appear uncharacteristic and unrelated.
What is Sjögren's syndrome ?
If selectively the production of aqueous tears is reduced by damage to the lacrimal gland, this is called Sjögren´s syndrome - for further details, please see below .
Therapy of Dry Eye Disease : → Timely and adequate treatment of the dry eye is important in order to avoid permanent damage to the eyes
The good news is that every patient can do a lot to improve the symptoms with a dry eye.
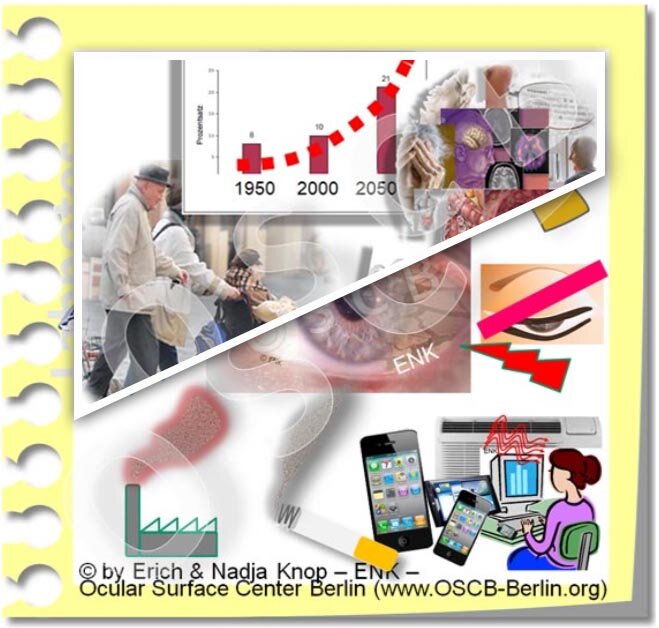
How common is the dry eye?
The dry eye is the most common disease in ophthalmology :
about 1/6 of the population is affected on average in Europe and North America
with about 1/3 of the population, the frequency of disease in Asia is about twice as high
with about 2/3 of the population in Asia, the frequency of Meibomian gland dysfunction is roughly twice as high as dry eye disease itself.
Meibomian gland dysfunction is the most common cause of dry eye, but it does not always lead to immediate complaints
the frequency of Dry Eye Disease is increased in certain conditions, e.g.
in women and
in advanced age
... this indicates an influence of hormones and aging processes.
Not every dry eye is recognized correctly, since the symptoms are often uncharacteristic at first and the onset is often gradual.
Complaints in Dry Eye Disease
What typical dry eye complaints ? - How do I recognize a dry eye?
The symptoms in Dry Eye Disease can be very different and therefore are often non-specific. Most dry eye complaints are due to eye irritation and tear film disorders:
Irritation and pain can be very different
wet eyes with tears running down over the cheeks
pain and chronic pain syndromes
Irritation and pain can be felt in different places:
Although the origin of the disorder is always on the front of the eye, the patient often perceives disturbing sensations or pain in various places:
on the surface of the eye itself
around the eye
on or behind the eyelids
occasionally even behind the eye
Disorders of the tear film can also lead to blurred vision and photophobia
For the reliable diagnosis of Dry Eye Disease, you should contact your ophthalmologist, who can investigate your condition more closely with clinical tests.
Gritty sandy feeling and itchy eyes
Gritty sandy feeling as if there were small foreign bodies in the eye and occasionally itchy eyes are common and annoying complaints in a dry eye.
The typical lack of tears or, more specifically, disturbed wetting of the surface, leads to poorer ´lubrication´ between the eyelids and the eyeball.
Poor lubrication creates an increased friction with all movements of the eye and especially with the frequent normal eyelid blinks that spread the tear film.
Any lack of tears will damage the surface of the eye !
The increased friction leads to constant small micro-injuries to the superficial cell layer on the eye, which causes subliminal pain. We take this as rubbing or as a gritty sandy sensation and, if it occurs constantly, also as a feeling of pressure.
Burning eyes and Dry Spots
A burning sensation is a typical complaint in dry eyes with an unstable tear film. A thinning and eventual rupture of the tear film causes "dry spots" on the ocular surface.
Dry spots can result in increased mechanical friction and increased salt concentrations. When tear water evaporates too quickly, there is a locally increased concentration of the dissolved salts and proteins in the tear film. This is referred to in the specialist literature as increased osmolarity/ hyperosmolarity.
Both, mechanical and chemical stress typically cause wounding of the cells and activation of adjacent nerve fibers which transmit signals to the brain. The patient perceives such signals as irritation or pain. 'Burning' is thought to occur particularly with hyperosmolarity. Mechanical and chemical stimuli can both trigger an inflammatory response.
Tired eyes, heavy eyelids, feeling of pressure and pain
The constant dryness and irritation of the surface of the eye leads to the sensation of ´tired eyes´, ´heavy lids´ or ´sticky eyes´.
Also, a feeling of pressure and pain may occur - this can be felt in very different locations: at the front of the eye or under the eyelids but also around the eye and even behind the eye. To further clarify whether it is really a dry eye, you should see an ophthalmologist !
Tired eyes, heavy eyelids and also a feeling of pressure can perhaps best be explained by the increased mechanical friction between the eyelids and eyeball with each of the numerous necessary eyelid blinks. As a result, the eyelids become 'heavy' and the frequent blinking with its constant irritation becomes tiring.
Sticky eyes and incrustations
A temporary increase in mucus production and possibly serous secretum from constant tissue wounding can lead to sticky eyes and to difficulties to open the eyes in the morning.
Deposits of altered oil on the eyelid margin in meibomian gland dysfunction or deposits from excessive growth of bacteria in case of chronic eyelid inflammation (blepharitis) can also contribute to adhesion.
If excessive mucous production and sticky eyes occur suddenly and severely, an ophthalmologist should be consulted to rule out a potentially dangerous infection
Deposits and incrustations on the edge of the eyelids and on the eyelashes occur in all forms of dry eye, particularly when this is associated with chronic eyelid inflammation (blepharitis).
The deposits contain inflammation-promoting substances that irritate the cell surface and can disrupt the tear film. This can make the disease worse. Regular and thorough eyelid cleaning with eyelid hygiene and care is therefore an important part of the treatment.
Visual disturbances, photophobia, sensitivity to glare
The thin and even tear film is disturbed in a dry eye. Since the tear film is not only important for moistening but also for good visual acuity, many patients have visual disorders such as
blurry vision, unstable vision
fluctuating visual acuity
glare sensitivity
photophobia
THERAPY → Visual disturbances in dry eye typically get better, or temporarily even disappear entirely, after one or more strong eyelids strokes that spread a new tear film. The new tear film is typically more stable because forceful blinking helps to express oil from the Meibomian glands in the eyelids and increases the thickness of the tear film lipid layer, according to studies.
Blink Excercise
Some vigorous eyelid blinks are also a good test whether visual disturbances are indeed caused by a tear film disorder (in dry eye) or whether a refractive correction (application/ change of spectacles or contact lenses) may probably be needed.
Wet eye and excessive tearing
Initially, the irritation of the ocular surface can lead to an increased flow of tears (as a protective reaction) ... with an overflow of tears (epiphora) over the edge of the eyelid.
It is, of course, confusing if the "dry" eye disease leads to excessive tearing and wet eyes.
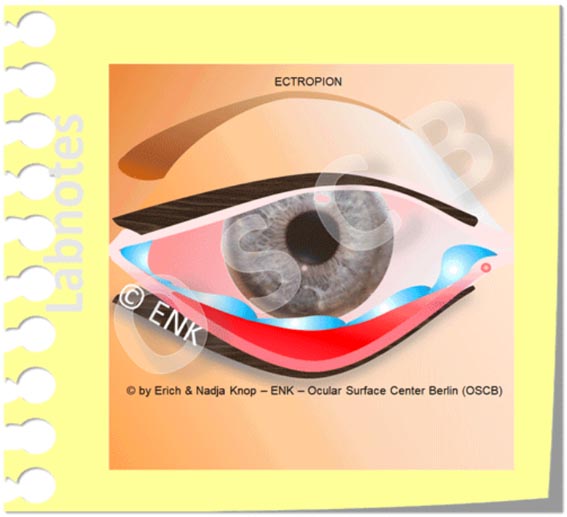
Other reasons for a wet eye and teardrops over the edge of the eyelid can be:
Changes in the shape or position of the eyelid, for example inward or outward curling of the eyelid margin.
Disorders of the discharge of tears into the nose. This may be occur either when the edge of the eyelid is everted from the eye globe or when the tear flow into or inside the nasolacrimal duct towards the nose is blocked.
THERAPY → Here, a close examination by the ophthalmologist and perhaps a small surgery can be useful.
Problems with contact lens wear begin or get worse
Contact lenses have increased demands on the tear film and increase the evaporation of the aqueous tears. Therefore, in dry eyes there is increasing intolerance to contact lens wear, especially of soft hydrogel contact lenses.
In addition, contact lenses cause increased friction on the eye. Therefore, according to studies, they contribute to changes in the surface of the eye that can favor a dry eye.
Many patients first try to compensate for the lack of tears with tear substitutes. However, this is usually not a recommended permanent solution for contact lens intolerance. It is better not to wear contact lenses at all, or at least not permanently, but to replace them with glasses.
Glasses are also beneficial for dry eyes because they offer some protection against drying draughts . If this is not sufficient, additional evaporation protection can be installed.
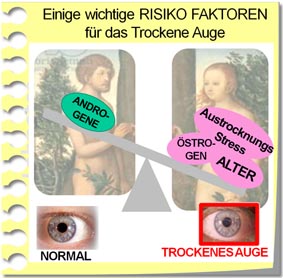
Risk factors for a dry eye
Many negative influencing factors are possible risk factors for a dry eye, for example:
( 1 ) Internal risk factors
In part, the risk factors lie in the body itself and are therefore difficult to influence:
Increased age leads to functional changes also at the surface of the eye
Disorders of the hormones occur naturally with increasing age
especially a relative lack of male hormones and an excess of female hormones were reported as risk factors for dry eye disease
this also applies to drugs such as anti-androgens and estrogen replacement therapy
Disorders of the eyelids and of the regular lid stroke/ blinking may occur with increasing age by changes in the eyelid tissue or may be caused by deregulation of the nervous system.
Previous eye surgery can cause or promote dry eyes
e.g. after removal of a cataract (cataract surgery) many patients notice a dry eye for the first time. Due to the very small surgery, however, it may be assumed that the dry eye already existed before and was just not noticed.
Refractive surgery or other operations that inevitably involve cutting many corneal nerves are known to typically cause dry eyes. However, this usually improves in the further course after the operation.
Chronic diseases and respective medication can also negatively affect the eye
especially if they disrupt the body's natural regulatory systems, which also regulate the eye
Nervous system (mental illness and also some respective drug therapies)
Hormone system (with increasing age, thyroid diseases, etc.)
Immune system (chronic inflammatory diseases)
various skin diseases (rosacea, atopic dermatitis etc.)
high blood sugar (diabetes) can make dry eyes worse
inflammatory rheumatic diseases and other systemic inflammatory diseases
Different drugs
which are administered to the eye as drops, especially when dripped permanently (e.g. to treat increased eye pressure / glaucoma)
or when medication is given systemically
e.g.: beta-blockers for high blood pressure, anti-histamines for allergies, and many other medications
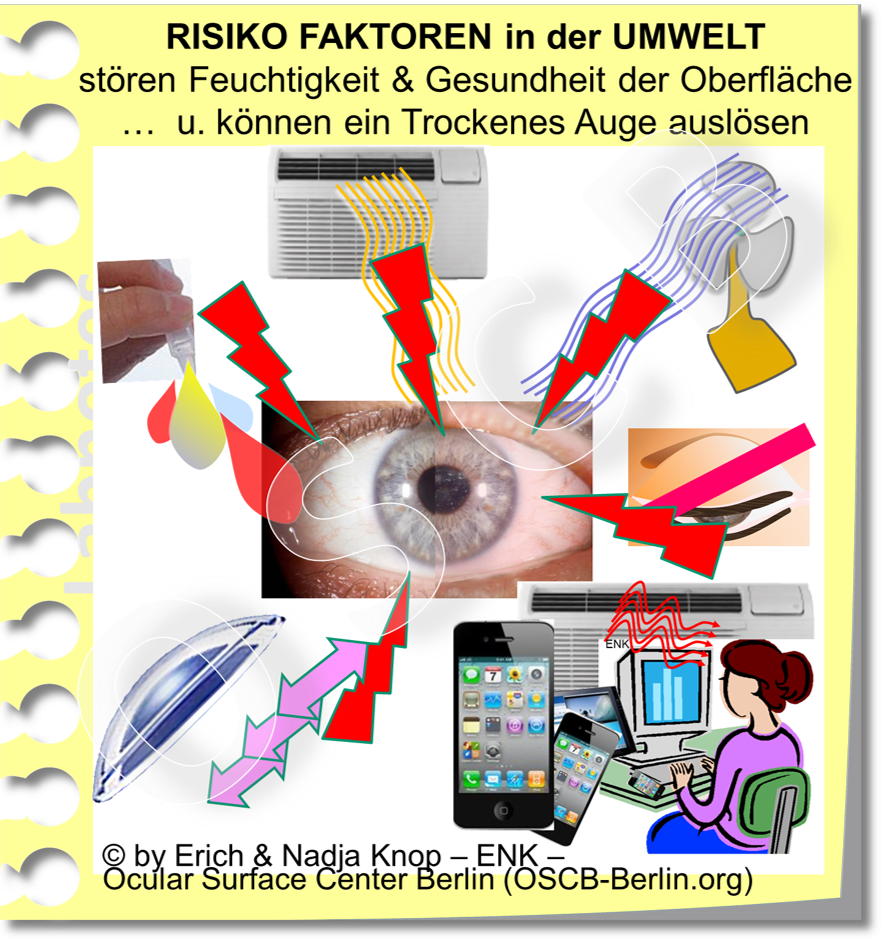
( 2 ) External risk factors
In part, the risk factors are outside the body, which typically offers a better chance to influence them into a positive direction.
Drying environmental conditions, such as those found in the natural environment, in homes and at many workplaces, may play an important role, e.g.
dryness, dry indoor air with further deterioration in winter in the heating season
airflow and wind from fans, air conditioners and blowers, for example when driving a car
as well as air pollution, smoke etc.
concentrated visual tasks - as such these external factors may trigger internal control errors (such as too rare blinking)
Cause of dry eyes
What is the cause of Dry Eye Disease ? - How does dry eye come about?
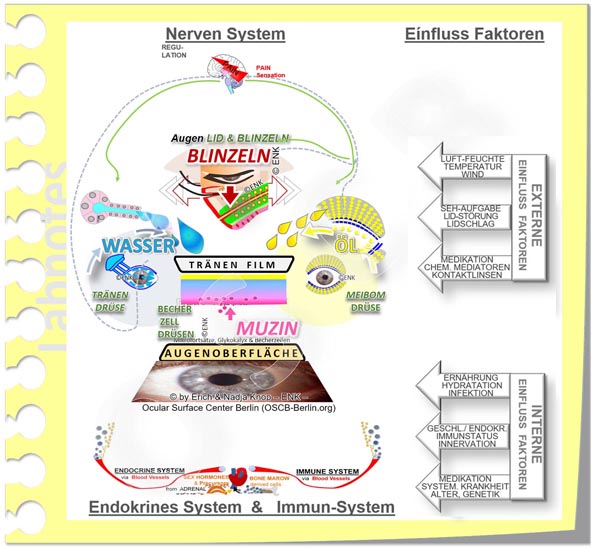
The decisive factor for dry eyes is a disruption of the Tear Film at the Ocular Surface !
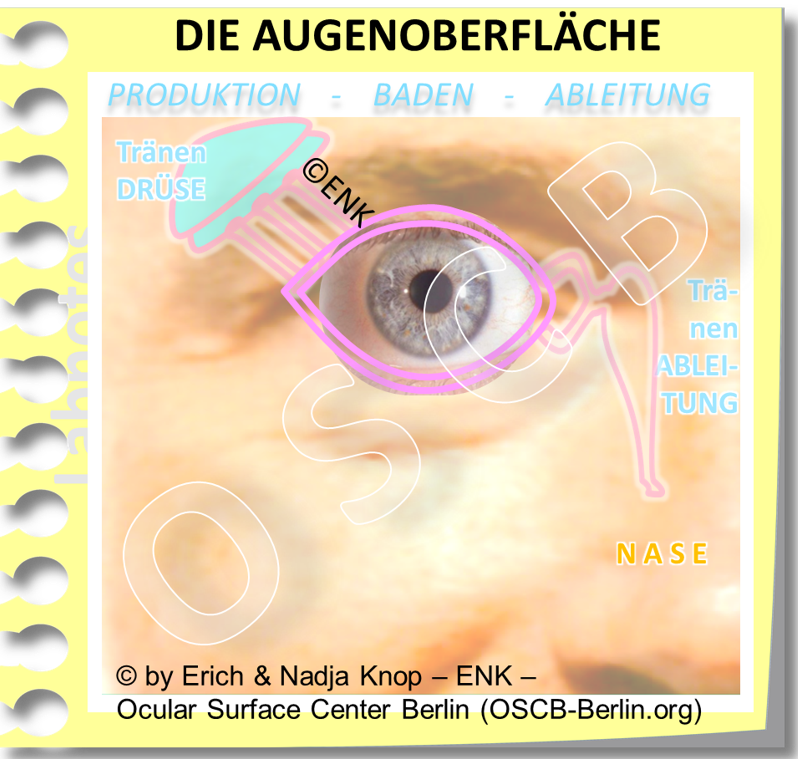
What is the Ocular Surface ?
The Ocular Surface consists of all the tissues and organs as well as the tear film that constitute the intact anterior surface of the eye and keep it constantly moist. This is a prerequisite for the health and function of the eye.
What is the Tear Film ?
The permanent moisture of the ocular surface is the ultimate pre-requisite for ocular health !!!
Therefore the surface is covered by a thin film of tears - termed as the tear film - to keep it moist even when the eyelids are opened to see the world around us !
The intactness of the tear film is thus of paramount importance for health and function of the eye ... we will therefore take a closer look at it below !
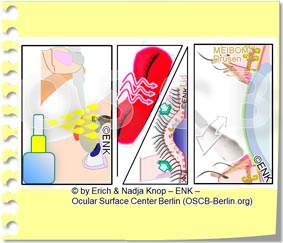
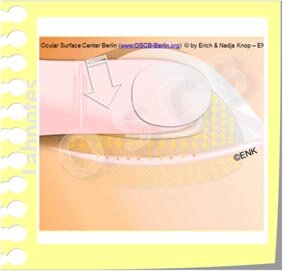
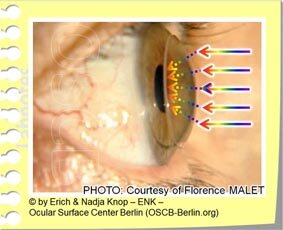
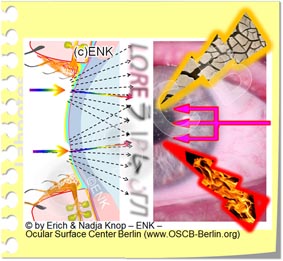
Schematic representation of the surface of the eye in cross-section. The blink of an eye forms the tear film from the tear fluid . Disorders of the regular blinking of the eye are a typical reason for disorders of the tear film and thus for a dry eye!
What are the tears - They consist of the secretions of the eye glands !
The tear fluid is produced by the glands !
… but tears alone are not enough to keep the eye healthy - the eyelids are equally important
WHAT is the tear film made of ?
it is a very thin and even layer of tear fluid on the eye
this wafer-thin tear film is still sufficient to keep the eye healthy and to create a perfect visual acuity.
it is understandable that desiccation is the greatest danger
HOW is the tear film made ? - The eyelids spread the tear film !
it is only possible by normal blinking of the eyelids
that the tear fluid on the eye within the opened interpalpebral cleft
is pulled out into a very thin and very even layer of liquid
The tear film is only stable for a short time - then it disrupts ! … and leaves the ocular tissue dry. The tear film
covers the surface of the eyes and keeps it moist while the eyelids are open to see
is only stable for a short time (about 10-20 seconds)
becomes thinner due to the normal evaporation of the tear water into the surrounding air atmosphere
develops ´holes,´ termed as ´dry spots,´ and finally breaks-up completely (termed tear film break-up)
therefore the tear film has to be renewed again and again with a new blink of the eyelids - roughly about 5-10 times per minute.
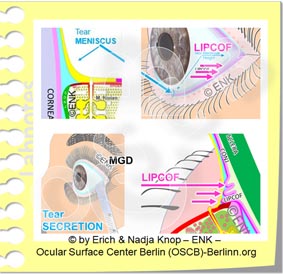
Where do the tears go to ? - they flow down into the nose!
With every new blink of the eyelids the ´old´ tears are sucked through the lacrimal punctum, that is on the nasal side of the upper and lower eyelids, and are directed to the nose .
What is the function of the tear film on the ocular surface ?
it keeps the tissue moist,
it ensures nutrition, regulation and health maintenance
it ´lubricates´ the sliding movement of the eyelids over the eyeball and all the voluntary movenents of the eyeball
it is the first and most important surface for the refraction of light - therefore the tear film is very important for a sharp vision.
even the smallest irregularities in the tear film, as they occur in dry eyes, lead to visual disturbances.
these visual disturbances typically consist of blurred vision. Since the vision fluctuates and usually improves temporarily after a few eyelid blinks, it is also known as “unstable visual acuity”.
How does dryness come about?
The dry eye is typically caused by a tear film disorder
A tear film disorder or deficiency leads to dryness of the eye. It can be caused by a deficiency
in the amount of tears produced by the glands ... or
in the composition and quality of the tears
A tear film disorder then leads to damage to the sensitive tissue on the surface of the eye.
Damage to the tissue surface occurs only rarely in first case in certain primary diseases … which may then secondarily disrupt the tear film.
Aqueous deficiency in the tear film ... can have various causes
Every dry eye has a lack of water … sooner or later
This creates a feeling of dryness, which is what gave the disease its name - even though patients can occasionally have episodes of wet eyes with excessive tearing, as explained above.
A lack of water can result from reduced production of aqueous tears by the lacrimal gland, e.g. in Sjögren's syndrome or in other, often inflammatory, disorders.
A primary lack of water due to a lacrimal gland disorder is rare however and, according to studies, only occurs in about 1/5 of the patients (Figure) .
Water loss due to increased evaporation of the available tear water on the surface of the eye is much more common, according to our current understanding. This occurs when there is a lack of oil and desiccating environmental influences.
This condition is termed as ´Evaporative Dry Eye”, is the main type of dry eye and occurs in approx. 4/5 of the patients.
THERAPY → Aqueous eye drops, with or without the addition of oil, are a useful therapy.
... they should be used as needed but often enough, up to every hour. An even more frequent application of watery eye drops is usually not sensible, as this can reduce the effect of your own (remaining) tears and may make the irritation of the eye even worse.
Lack of water ... in Sjögren's syndrome is caused directly by alteration of the lacrimal gland
Henrik SJÖGREN, Swedish ophthalmologist, who was the first to describe the inflammatory disease of the tear and salivary glands named after him, which leads to the Sicca syndrome of the eyes and mouth.
The so-called Sjögren´s syndrome is a special form of aqueous tear deficiency, but it is very rare.
It arises from a chronic auto-immunological inflammation of the tear glands of the eye and also of the salivary glands in the mouth. This was first described by Henrik Sjögren in 1933.
Chronic gland inflammation causes dryness of the eyes and mouth - typically with inflammatory swelling of the glands. It can occur together with auto-immunological rheumatic diseases and skin diseases.
Sjogren´s syndrome is very rare with an incidence of well below 1% of the population. It typically leads to a severe lack of aqueous tears up to the complete absence of tears.
Therefore, not every lack of aqueous tears is caused by Sjögren´s syndrome and a suspected diagnosis must be confirmed accordingly by a clinician, for example by detection of autoantibodies in the blood.
Oil deficiency ... is the main reason for tear film deficiency - it mostly arises from dysfunction of the meibomian oil-glands inside the eyelids
The meibomian oil glands in the eyelids usually (left) form oil for the tear film, which inhibits the evaporation of the tear water. If the oil glands are clogged (right), the tear water evaporates quickly and the eye becomes dry.
It is usually not the water of the tears that is missing first, but the superficial layer of oil on top of the tear film, that has the function to reduce the evaporation of the water.
The oil comes from the Meibom oil glands in the eyelids:
the amount of oil is quite small compared to the aqueous tears from the lacrimal gland.
therefore, a lack of oil practically does not change the total amount of tear fluid, only its quality - but this is already sufficient to disrupt the tear film.
Oil deficiency is caused by a disorder of the Meibomian glands inside the eyelid, termed meibomian gland dysfunction ( MDD).
Usually the glands are clogged, then oil is missing and the aqueous tears evaporate faster leading to a subsequent dry eye. Meibomian gland disorders are very common and increase with age.
If the meibomian glands are blocked, there is not only an oil deficiency with a dry eye but also unnoticed damage to the glands inside the eyelid due to the increased pressure that develops in the blocked glands.
THERAPY → Eye drops that contain oil or a lipid spray can help here acutely to compensate for the lack of oil on the tear film ... but ...
... above all, it is important to improve the function of the oil-producing meibomian glands inside the eyelids ! This is done by physical lid therapy (with warming, massage, cleaning), which the patient himself regularly carries out at home.
Further therapy options for meibomian gland dysfunction (MDD) and for the often associated blepharitis / eyelid inflammation can be found → here
Disorders of the eyelids and of blinking prevent the tear film from spreading normally
Incomplete blink of an eye
The eyelids are important for the health of the eye
Regular blinking is necessary:
to draw the tears into the thin tear film on the eye and
to squeeze small droplets of oil from the meibomian glands to retard water evaporation and to make the tear film more stable
Eyelid disorders contribute to dry eye
( 1 ) Changes to the eyelid itself in shape and position can alter the normal blink of the eye and thus the spread of the tear film for moistening - this can contribute to dry eyes.
Changes of the eyelids occur more often with increasing age without being noticed
The shape of the eyelids can also change after injuries and accidents
( 2 ) Disorders in nerve regulation of the eyelids or habitual disorders of blinking are of underestimated importance:
Rare blinking and incomplete blinking are common causes of a tear film disorder.
If rare blinking occurs, the tear film is not renewed often enough - it breaks-up and the eye becomes dry, which leads to irritation and visual disturbances. The normal frequency of blinking is about 5-10 lid strokes per minute - but this is highly dependent on the current visual task.
With incomplete blinking / " nervous blinking " the eye is not completely closed and only the upper part of the tear film is renewed - the lower part of the ocular surface remains dry (please see figure). Therefore the first and most frequent ocular surface damage can be found in the lower part.
" Office Eye " combines many risk factors
The so-called Office Eye is a rapidly increasing form of dry eye in "modern" office work environments. Several harmful influences can add up here and may thus quickly lead to a dry eye condition. This form of dry eye not only affects the elderly, but is also increasingly common among younger people .
Concentrated visual work (e.g. computer screen, television, driving a car) is accompanied by rare blinking and may therefore easily lead to a dry eye.
The risk of a dry eye increases:
in a dry environment (air conditioning) and / or
with draughts (fans/ blowers) and / or
dust particles or smoke in the air, as well as
mental stress and additional
too little drinking volume
In ´Office Eye´ condition an unstable tear film occurs in addition to desiccating environmental factors and perhaps negative internal influences on tear production, such as e.g. mental stress.
THERAPY → Own observation of your blinking habits and, if necessary, changing of the blinking pattern is important for a sufficiently frequent and complete blinking. Normal Blinking is a basis for ocular surface health !
In addition, conscious blink exercises can be useful at work - there are even computer apps to remember.
Avoiding work environments that are too dry, taking sufficient breaks and drinking enough water is also helpful - please consider 7 golden rules for improving eye health .
What damage is caused by dryness ?
Deficiency and disruption of the tear film leads to tissue damage ... and vice versa
Every tear film deficiency causes tissue damage to the surface of the eye - regardless of whether this is due to increased evaporation or a primary decrease in aqueous production by the lacrimal gland or an oil deficiency due to Meibomian gland dysfunction.
Tissue damage leads to poorer wettability of the tissue at the ocular surface and thus increases the primary tear film disorder.
Tissue damage also triggers irritation of the sensitive nerve fibers and thus irritation and pain.
=> Tear film disorder and tissue damage influence each other negatively and thus form a central ´vicious circle´ of self-aggravation in dry eye disease that makes everything worse. In addition, there are many more such negative mechanisms.
Furthermore, the tissue injury leads to the development of inflammatory processes.
Inflammation is a defense reaction of the body - however, in chronic disorders, as is the case with dry eyes, chronic inflammation can lead to an intensification of the disease process.
Irritation, pain, and chronic pain syndromes
Dryness with increased friction on the eye and increased concentration of salts (hyperosmolarity) in the remaining tears leads to tissue damage.
Tissue damage also causes irritation of the nerve fibers, which are very numerous at the surface of the eye.
The different complaints that can be felt in different regions of the eye indicate that dry eye disease leads to a complex alteration of the nervous system.
Persistent eye irritation can cause pain, and chronic pain can lead to a disorder of the pain system. Chronic pathologic pain syndromes may then develop. They can be an important factor in dry eye disease and are often difficult to treat.
A collaboration with pain medicine, psychosomatic medicine and neurology, can be helpful when strong subjective symptoms of dry eye disease are present without significant clinically apparent damage. At the same time, these patients sometimes also have other functional disorders of a psychosomatic type (such e.g. as irritable bowel syndrome, unclear spinal syndromes, tinnitus, unclear dizziness, etc.) which may help do diagnose the condition.
What causes worsening of dry eye ?
The "dry eye" tends to worsen without adequate treatment
When does a dry eye turn into dry eye disease ?
A 'dry' eye can also occur in a healthy person, once in a while - but if it becomes chronic, it can turn into a disease
Occasional dryness of the eyes can sometimes occur- even in healthy people. It usually improves quickly after a few vigorous eyelid blinks and when risk factors are avoided. Only when the condition occurs chronically can an occasional "dry" eye develop into the "disease of the dry eye”, which is simply termed as ´´Dry Eye Disease´.
"Vicious Circles" of disease worsening
Tear disorders
A tear film disorder creates or worsens the irritation of the ocular surface.
Irritation
An irritated ocular surface in turn makes it more difficult for the aqueous tears to stick to the damaged cell surface and thus deteriorates the stability of the tear film (please see figure ).
"Vicious Circles"
Therefore, tear film deficiency and surface damage in dry eye disease tend to reinforce each other. The pathology in dry eye disease thus tends to get worse if there is insufficient treatment.
Such self-reinforcing reactions are referred to as ' vicious circles' of disease aggravation.
Inflammatory reactions accelerate the self-aggravation of dry eye disease.
=> HERE is a detailed description of the pathophysiology of Dry Eye Diseease
Inflammation accelerates the dry eye disease process
If the surface of the eye is permanently irritated and wounded, as is typical for dry eye disease, this can trigger an inflammatory reaction.
An inflammation is actually intended to defend the eye. If it becomes chronic, however, it can become a disease factor.
If the inflammation persists chronically, it makes the dry eye worse.
Therapy: Anti-inflammatory therapy by the ophthalmologist can be useful here.
The ophthalmologist you trust and, for difficult cases, also specialized centers for Dry Eye Disease have more therapy options available.
In the case of a severe dry eye, the functional circuits of an intact ocular surface are increasingly destroyed.
Increasing tissue disorder develops. This reduces the wettability of the surface and the production of tear fluid by the glands for wetting.
The constant irritation of the nervous system not only triggers chronic irritation and pain, but also reduces the regulation of gland activity.
Furthermore, the increased friction and irritation on the eyelid margin increases the dysfunction of the meibomian glands and the development of chronic eyelid inflammation (blepharitis).
Increased friction, reduced wetting and inflammation of the cornea can damage the constant regeneration of the top corneal layer (epithelium). This can cause vascular ingrowth and clouding of the cornea .
Therapy
There are many therapy options for Dry Eyes
Therapy: An interruption of the harmful vicious circles of self-aggravation can be aimed at by:
adding up the tear fluid with aqueous eye drops (tear supplements), with and without oil, or by
gels or ointments overnight
physical lid therapy for the eyelids to improve the meibomian gland function and
cleaning of the eyelid margins from inflammatory depositions
Your ophthalmologist can recommend other options for the what you can do for the detection and treatment of dry eye and as a specific therapy for dry eye disease.
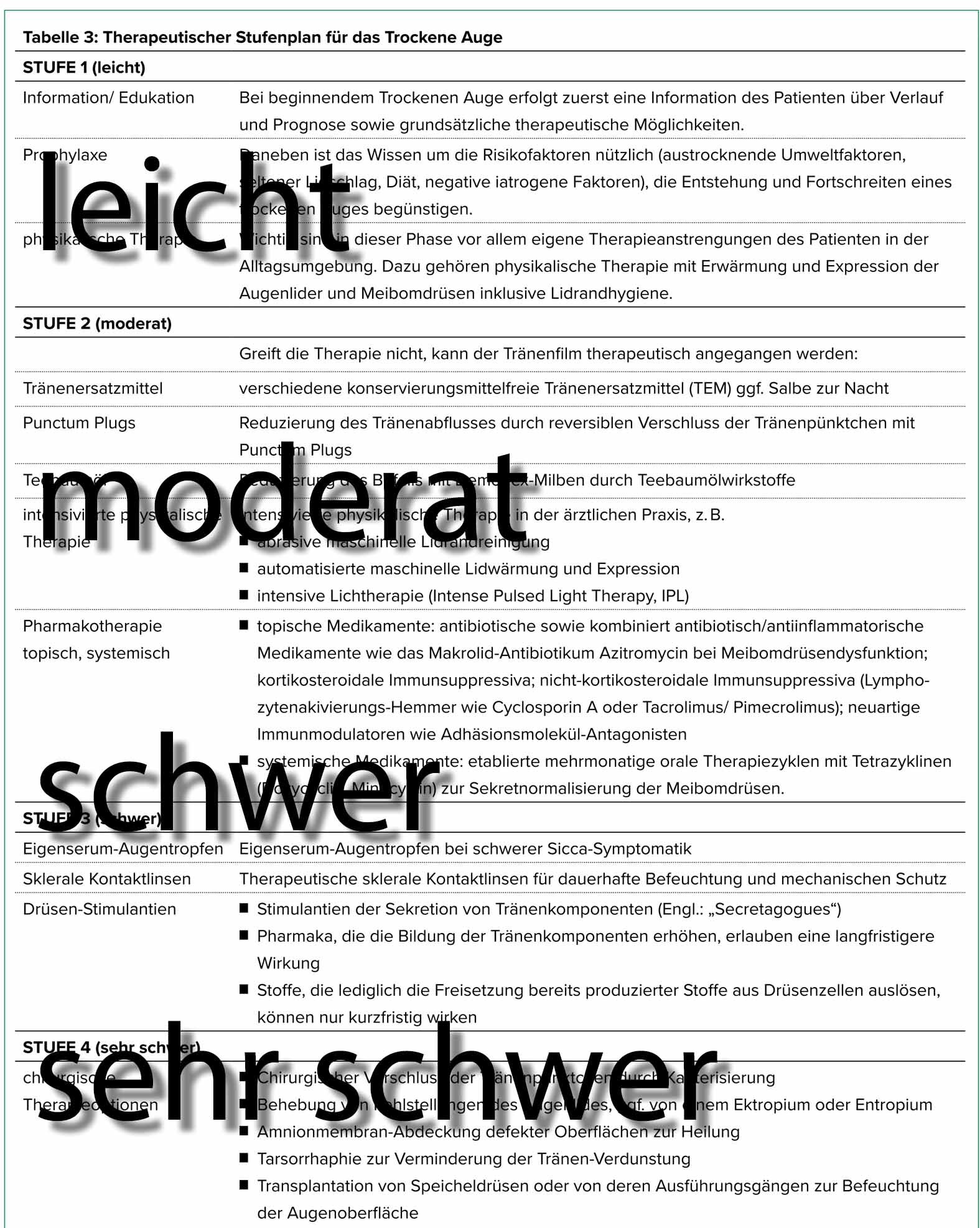
Typically, a step-by-step therapy is performed after a review of your medical history and a thorough diagnosis of the causes.
With step-by-step therapy, the treatment is intensified depending on the severity of the disease until a sufficient improvement is achieved.
DRY Eye
WET Eye
and the EYELIDS

=> BACK to PAGE selection for FACTS
Dry Eye, Wet Eye & Eyelids
Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT ]
On this page you will find the following TOPICS for selection by clicking on an image
.
Irritated eyes - dry eyes - watery wet eyes - eye rubbing - foreign body sensation - burning eyes - red eyes - tired eyes - glued eyelids - blurred vision - unstable vision ... and much more ....
All of these apparently very different, uncharacteristic symptoms can be signs of eye irritation due to damage at the surface of the eye.
This bundle of various dry eye complaints explains its named as “ Sicca syndrome ”
Typically, it is caused by a lack of the tear film on the eye. It can then no longer keep the sensitive tissue sufficiently moist, intact, and healthy. The typical result is a local or general tissue damage, mainly by drying, together with irritation - hence the term "DRY EYE".
Also a wet eye, however, with increased watery lacrimation can be based on or go along with a lack of normal, sufficient and even wetting and thus with a lack of normal tissue protection.
The so-called "DRY EYE" does not always have to be dry
In contrast to its designation as "dry", the irritation of the eye can also lead to episodes of increased lacrimation and thus to a 'wet eye´. This occurs especially at the beginning of this disorder and often in elderly people ... this counter-intuitive observation often seems difficult to understand for patients.
Doctor, my eyes are WET ... how can that be a 'DRY EYE'?
An increased tear flow may be due to a (still) intact defense reflex of the eye.
In the event of irritation of many kinds, e.g. airstream, ventilators, dusty air, or foreign bodies, etc., the defensive reflex ensures that the tears flow strongly to 'flush away' the source of irritation.
If the damage to the surface of the eye has progressed, the nerves will also be damaged.
Then, unfortunately, this protective reflex also stops and the excessive tearing of the eyes disappears ... which is not a good sign in the end.
Other reasons for a “Wet Eye“
A “Wet Eye“ can, however, also have other reasons than increased production of tears. An impairment of tear discharge of ´used tears´ from the eye into the nose may also result in wet eyes. It can occur e.g. due to an altered eyelid shape and function or due to a blockade of the outflow system.
Wet Eye with Blockade of tear outflow and infection - See an Eye Doctor !
Occasionally a blockade of the tear ducts, that drain the tears from the eye into the nose, may be responsible for watery eyes. This goes typically along with bacterial infection and pain and needs timely effective therapie.
=> Therefore, every ´wet´ eye should be seen and diagnosed by an ophthalmologist !
Blurred vision can also occur in a wet eye
The moisture of the tear fluid is necessary to keep the ocular surface healthy - but it is not sufficient to produce perfect vision.
When the thin tear film is inhomogeneous the visual acuity is reduced and typically unstable or fluctuating. This occurs when tears are
too low ... as we can see by a lack of tears in Dry Eye Disease but also
too high, as occurs by an overflow of tears in patients with episodes of excessive tearing in Dry Eyes and in emotional tearing (crying).
So, the volume of tears alone is not sufficient but a thin and homogeneous tear film is necessary.
Blurred vision can thus occur in dry and in wet eyes !
Healthy eyelids are very important for a healthy eye
The eyelids have several important functions for maintaining health at the surface of the eye.
most obvious is probably that the eyelids can close and protect the eyes
the eyelid blink spreads the tears into the tear film, similar to a wind-screen wiper.
the tear film provides the moistening and a sharp vision
the oil glands in the eyelids release oil at the blink so that the aqueous tears do not evaporate so quickly
the eyelid blink also maintains the discharge of ´used tears´ from the eye into the nose.
Changes in the eyelids can lead to a wet eye with excessive tearing
Protruding lower eyelid with curl of the lid edge outwards (ectropion)
Eyes with disturbed eyelid position or with a disturbed function of the eyelids can no longer build up a normal tear film or can no longer hold it on the surface of the eye.
Therefore, a disturbed eyelid position can occasionally be the reason for wet eyes with overflowing of tears over the edge of the eyelid and cheeks - medically known as epiphora.
In addition, the tears can often no longer be pumped normally into the nose due to the change in the eyelid, so that the tears overflow over the edge of the eyelid.
Although the eye is moist, the tears cannot form a stable tear film. This leads to a "dry eye" type of of ocular tissue irritation.
Due to the subsequent irritation of the nerve fibers, even more tears are produced (irritant stress secretion) - However, these tears consist mainly of pure water and therefore cannot form a stable tear film and cannot adequately lubricate the tissue.
Causes of eyelid changes
Rolling the edge of the lid inwards (entropion) with rubbing of the eyelashes on the eye
A disturbed eyelid position can result from
Relaxation of the connective tissue or also
due to scar tissue, e.g.
due to an accident or
Here, urgent medical advice should be sought!
Consequences of eyelid changes
Eyelid disorders can lead to
Protruding lower eyelid with outward curling of the lid margin (ectropion) or
Inward curling of the edge of the eyelid (entropion), often with rubbing of the eyelashes on the eyeball and severe irritation.
Disturbance of nerve regulation can also be important
Distrubance of nerve regulation can impair a normal eye blink even when the eyelids have a normal shape and position.
The DRY EYE is a "tricky" condition of the surface of the eye
It becomes clear that the so-called ´Dry Eye´ is a very ´ tricky ´ disorder of the eye.
In order for the surface of the eye to function healthily, many factors must work together. This may be comparable to a house of cards that looks quite stable ... but as soon as only one card is moved ...
It is TRICKY …
that a ´Dry´ Eye can frequently be wet and watery, at least in the beginning and in episodes
that a Dry Eye typically first lacks oil and not water, as could be assumed
that the mere amount of tear fluid is not sufficient for a healthy eye - because the thin Tear Film on the eye is the ´tip of the scales”
also the ´quality´ of tears must be right, i.e. the composition must be sufficient, e.g. enough oil but also other factors are important
and the eyelids must function properly
… and … and … and …
Science is been intensely working on the treatment and potential elimination of this disease for a long time. Considerable progress has been made, which benefits hundreds of millions of patients worldwide ...
It is crucial for the patient to understand his/her disease - there are many ways of improving the condition by themselves.
If you want to learn more about it … this is the right place for you
on the information portal of the ´Ocular Surface Center Berlin´ (OSCB) - the research center for the ocular surface and for dry eye disease.
Please choose a topic according to your interest ...
- or just follow the presentation on this page ... which is perhaps the most informative
QUICK
GLIMPSE
on Dry Eye Disease
Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT ]
Quick GLIMPSE
The ´ PATIENTS´ Page ´ on Dry Eye Disease
… will not dig too deep
but will explain interesting facts ... generally understandable !
Moisture comes from tears and is produced by the eye glands.
The tear fluid must be distributed to the thin tear film on the eye by the blinking movement of the eyelids ... to make the moisture permanent - always and everywhere ... and to allow perfect visual acuity.
Oil from the Meibom oil glands in the eyelids ensures that the tear film remains stable for longer.
If one of these conditions is disturbed, it can lead to dry eyes. They are based on a disturbance of wetting with subsequent damage to the surface tissue.
The lack of tears is usually caused by increased evaporation of the watery tears. This in turn is caused by a lack of oil on the tear film when the eyelid oil glands are blocked.
Dry eyes are promoted by numerous negative risk factors, which are partly in the body and partly in the environment. This opens up many possibilities for prevention, improvement and treatment of the disease.
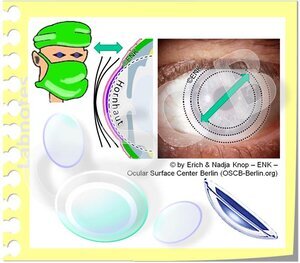
Contact lenses can contribute to dry eyes ... but speciality contact lenses can in selected cases also help with severe dry eyes
Please select a TOPIC of your interest by clicking on an image
- or just follow the presentation on this page ... which is perhaps the most informative
The surface of the eye
The ocular surface ... is the moist frontal part of the eye
It mainly consists of the clear cornea in the middle and the supporting tissue of the conjunctiva around it, which actually forms most of the ocular surface tissue (please see animated image).
The ocular glands and their secretions (tears) as well as the eyelids that spread the tears into the tear film are certainly also part of the ocular surface.
The cornea
is the clear tissue in the middle
it serves for the transmission and refraction of light
even though it may remind of a simple piece of ´plastic´ it is in fact a very delicate and highly specialized tissue that needs careful attention !
The conjunctiva
covers the eyeball from the front, where it lies on the hard eye wall (sclera),
then turns over and covers the eyelids from behind
thereby it forms the conjunctival sac
occasionally, foreign objects can get into the conjunctival sac (which is very irritating) and are then best rinsed out.
is the main support tissue for the cornea and helps to keep the cornea moist etc.
contains the blood vessels that are seen on the eye and can be moved with the delicate flexible conjunctival tissue
when the eye is irritated the conjunctival vessels fill up and cause the typical reddening.
The gloss on the surface of the eyes is created by moisture of the tear film, which ensures that the mucous membrane remains constantly moist - even with opened eyelids.
The tears consists of the fluid secretions from the various glands, that are somewhat hidden and also belong to the ocular surface.
The eyelids protect the moist mucous membrane and distribute the tear fluid into the tear film.
=> here you will find more in-depth information about the surface of the eye.
The surface of the eye ... allows the first steps of Vision
The surface of the eye is that part of the eye through which the light enters.
Only then can the light trigger stimuli on the retina in the back of the eye, which can later be processed into an image of the outside world in the ' curious' brain.
Without a healthy eye surface, all functions of the visual process that are further back and later are ultimately relatively meaningless for vision.
Tears - the magic juice that keeps the ocular surface healthy and going
Tears are the ´magic juice´ that serves for many, many, many purposes the ocular surface.
They are produced by different glands and consist of different substances. Tears also contain some substances from the blood.
The function of tears does not only serve for wetting of the tissue surface but also maintains e.g.:
lubrication and thus reduction of mechanical friction
regulation of growth, regeneration and wound healing of the tissue
protection against infection
oxygen transmission
… and many more functions
Wetting is probably the most obvious function of the tears and dry eye disease is based on a wetting deficiency. Therefore, (mainly aqueous) tear supplements have occurred as the most obvious from of therapy.
The moisture of the tears comes from the glands of the eye
The tear fluid is produced by several glands.
Three different types of glands are needed because the tear film on the eye is made up of three different main types of substances:
Water ... is the main part of the tears and comes from the lacrimal gland behind the upper eyelid at the outer top of the eye socket. Several small accessory lacrimal glands contribute smaller amounts of fluid.
Oil ... from the meibomian glands can reduce the evaporation of the water. Oil forms a thin layer on the surface of the tear film. The meibomian glands are elongated strands in the eyelids, They can be seen at the inside of the lower lid when it is slightly everted.
Mucus (a slimy substance composed of mucin molecules) ... mainly comes from individual small goblet cells that are distributed along the conjunctival sac (see pink dots in the figure). The mucus is needed to bind the water of the tears to the cell surface.
The various glandular products are arranged in layers in the tear film on the eye.
Tears flow along the surface of the eye
Tears are produced by the various glands on the surface of the eye.
Most of the volume consists of water and comes from the lacrimal gland, that is located at the outer upper aspect of the eye socket behind the upper eyelid.
From there, the tears enter the conjunctival sac. The tears flow towards the nasal side of the eye. This occurs behind the eyelids and along the lid margin in the lacrimal strip (tear meniscus).
Through the blink movement of the eyelids the tears are spread into the thin tear film over the visible frontal part of the eye and keep the tissue moist.
On the nose side, the ´used´ tears are then sucked up by small holes (lacrimal puncta). One punctum each occurs on the nasal side of the upper and lower eyelids and they dip into the lacrimal strip.
Tears reach the nose through the draining tear ducts (please see animated figure). When larger quantities of tears get there, e.g. when crying, they can run into the throat, where we can notice their salty taste.
Alterations of eyelids or a blockade of the nasal outflow, often with bacterial infection, can both cause a ´wet eye´ with overflow of tears over the edge of the eyelid.
The meibomian glands are of particular importance for the surface of the eye
The meibomian glands in the eyelids produce oil for the tear film
Meibom oil protects the tear water from evaporation .
The meibomian glands form long strands in the eyelids. They produce lipids/fats that are liquid at body temperature and thus form an oil.
Meibomian glands are of particular importance for the health of the ocular surface because their oil retards the evaporation of the watery tears.
In the dry environment we live in, the watery tears evaporate faster from the surface of the eye than the lacrimal gland can produce them. We therefore need an oil layer on the surface of the tear film to sufficiently inhibit evaporation.
A lack of oil on the tear film and/or environmental factors that increase evaporation … will both favour a dry eye condition.
A lack of oil on the tear film is the main primary cause for dry eye disease, particularly in elderly individuals.
Desiccating environmental factors often occur in office environments and cause dry eyes in many younger individuals.
The blink movement of the eyelids ensures the squeezing of the meibomian glands
The blink of the eyelids ensures that the meibomian glands are squeezed out: the meibomian glands form the oil through piles of glandular cells in rounded end pieces (“secretion” at the bottom left of the figure). The glandular cells lie deep in the eyelid and fill the duct system of the glands with lipid secretum (arrows). The light pressure of the eyelid muscles, upon the blink of the eyelids, pushes oil droplets out of the gland opening at the edge of the eyelid (“Dellivery”).
The power of muscle contraction when blinking contributes to squeezing meibom oil out of the glands, increasing the thickness of the oil layer on the tear film
Rarely blinking is therefore an important cause of an oil deficiency on the tear film and may be a co-factor for the onset of meibomian gland dysfunction (MDD).
Deliberate, forceful blinking helps, according to studies, as an easy way to increase the oil layer on the tear film and thus increase the stability of the tear film and avoid or improve a dry eye.
The eye surface must be constantly moist
The surface of our eyes is a mucous membrane. It is constructed in such a way that it has to be permanently moist - ´everywhere´ - so that it stays healthy and that the cornea, the clear window of the eye, remains really clear.
This moisture is produced by the glands on the surface of the eye and is known as tears *.
Since we live in a dry environment with an air atmosphere, it is very difficult for the eye to maintain this small, artificial, moist "ecological niche" on the surface of the eye - "Always and everywhere"!
* In addition to keeping the ocular surface moist, we can also use the tears to convey the emotional signal to our fellow human beings that we are particularly sad ... or particularly happy - Hmmm ... doesn't it say 'tears don't lie'? ... but with that we leave the sure ground of science and therefore do not pursue it further!
The eyelids and blinking are just as important as the tears
A sufficiently frequent and complete blinking is necessary for an even and stable tear film.
a blink mainly moves the upper eyelid down, and wipes over the cornea and conjunctiva
when wiping down the ´old´ tear film is ´ cleared away´ (into the lacrimal tear strip) - and the tears are sucked into the lacrimal puncta and transported to the nose.
a new tear film is spread out when the upper eyelid is opened
The tear film is a ´trick´ of the eye for moisture and vision at the same time
Moisture "always and everywhere" presents a problem to the surface of the eye, or, to put it more nicely, a challenge :
Only when the eyelids are open can light enter the eye ... but then the surface of the important cornea would begin to dry out immediately. Therefore, the eye has a ' trick ' access:
A thin layer of tear water - called the " tear film " - is formed, which is thick enough to keep the cell surface moist , but thin enough not to disturb the entry of the light!
Another important effect of the tear film is that it fills all ´unevenness´ of the surface and thus creates a perfectly smooth surface for a perfect refraction ... for a perfect visual acuity !
Since only the regular blinking of the eyelids can produce a stable tear film, the eyelids and their blinking are just as important as the production of the tear fluid.
The Tear FILM is the solution for all 'Problems' on the ocular surface ... and for the SEEING
The tears are transformed into the important thin tear film.
This happens through the orderly blinking, i.e. the wiping movement of the eyelids over the surface of the eyeball.
Only by blinking and the special composition and arrangement in layers of the tear film it becomes possible to produce a very thin (about a hundredth of a millimeter) tear film.
The tear film must remain stable at least until our curious brain has a sufficient picture of what is going on in the environment. The tear film should remain stable for at least 10 seconds until it breaks up.
The ´break-up´ of the tear film is then the stimulus to trigger a new blink of an eye, which spreads a new tear film.
The tear film forms a thin and even coating on the surface of the eye
View into the tear film
The surface of the ocular cells is covered with a thin, even coating of tear fluid - the tear film. For the adhesion of the watery tears serve water-binding mucilages (mucin molecules, in the figure indicated as pink fibers). Some are attached to the cells and others are dissolved as a gel in the water of tears. In addition, the cells have numerous finger-like extensions that enlarge the surface and thereby improve the adhesion. If the normal cell surface is damaged, the binding of the tear film to the tissue surface is reduced and it breaks up quickly.
The tear film is arranged in layers
The tear film coating is distributed on the surface in a layer-like stucture by the eyelid blink movement of the lids. The layers are not sharply separated but instead mixed to a certain extent. Each layer of the tear film consists mainly of the secretions of one type of gland.
the bottom layer is formed from the mucilage (mucin molecules, shown as pink ribbons in the figure). They bind the watery tears to the cell surface and thus maintain wettability of the tissue surface.
the middle main layer of the tear film consists of the water of the tear gland, which together with soluble mucilage forms a water-mucin gel . This is used for ´ lubrication ´, that is, to reduce the friction between the eyelid and eyeball during frequent eye flaps. In addition, the tears contain numerous important substances for keeping the tissue healthy.
the surface layer is very thin and consits of the oil (yellow in the picture) of the meibomian glands, which are located in the eyelids. The main function of the lipids in the oily layer is to reduce the evaporation of the watery tears. If oil is missing, evaporation increases and dry eye can easily develop.
Only a thin and even tear film allows perfect visual acuity
An intact, thin and even tear film is not just for moistening of the ocular surface.
It is also the prerequisite for perfect refraction and therefore good visual acuity.
Tear film disorders typically lead to decreased or fluctuating visual acuity
In principle, everything is already said:
The basic requirement for health and visual acuity is a stable tear film that is created by the
Production / secretion of tears through the eye glands and the
Formation / spreading of the tear film by eyelid blinking
... and if the conditions for keeping moist are disturbed or the tear film dries out due to external factors - then there is a dry eye !
DRY-EYE-DISEASE
… after the moisture is gone
When there is no (sufficiently) stable tear film, the eye will dry up !
How does a dry eye show up?
Blurred Vision and Eye Irritation occur when the tear film breaks-up
Development of a ´dry spot´in the tear film due to tear film deficiency
The tear film only has a limited 'durability' of approx. 10-20 seconds - this is called ´tear film stability'.
Therefore, the blink of the eye must be repeated frequently - about every 10 seconds or about 5-10 times a minute - to spread a new tear film with every blink.
If the tear film is not renewed in time, it locally becomes thinner and breaks-up (see animated figure). The resulting ´dry spot in the tear film´ has 2 consequences:
the refraction of light becomes irregular and the visual acuity becomes unstable or blurred. This is often an early indication of a dry eye.
the tissue begins to dry out immediately.
this triggers irritation of the nerve fibers located there and thus induces a new blink or increased tear flow.
repeated irritation leads to symptoms of eye irritation that are known to all patients.
chronic irritation can also lead to pain and can possibly develop into a pain syndrome
Damage to the tissue surface results from disorders of the tear film
When the tear water evaporates (blue wavy arrows), the salts and proteins (grey circles in the liquid) remain and cause a more concentrated "salty" composition of the remaining tears, called "hyperosmolarity". Hyperosmolarity, similar to increased mechanical friction, irritates eye tissue and cells. This leads to damage and inflammation in dry eye disease.
All disorders of the tear film lead to damage to the tissue on the surface of the eye.
First the water-binding layer of mucus (indicated pink in the figure) at the bottom of the tear film is damaged and later the numerous small finger-like cell extensions are damage or lost. Both are important for the ability of the surface to bind water.
When the wetting is thereby disturbed, the tear film becomes unstable and breaks-up easily. This creates gaps/ holes in the tear film, termed as dry spots.
Dry spots in the tear film increase the mechanical friction during movements between the eyeball and eyelid, e.g. during regular eyelid strokes. This causes further damage.
If evaporation of the aqueous tears increases the salt concentration in the remaining tears (increased osmolarity/hyperosmolarity), this leads to damage through dehydration and cell shrinkage (see animated figure).
The osmolarity of the tear film can nowadays be measured relatively easy.
Increased mechanical friction and increased salinity of the tears (hyperosmolarity) puts the cells into an 'alarm state' and can trigger further reactions such as an inflammatory reaction - an important reinforcement mechanism in dry eye.
Later there are gaps in the cell layer and the tissue shows degenative remodelling leading to a loss of function.
Rarely, the tissue at the surface of the eye is damaged first, with a later secondary disorder of the tear film and moistening.
Tear film disorder leads to tissue damage, irritation, inflammation and pain
Tear film deficiency with damage to the surface of the eye and irritation of nerve fibers triggers the typical findings of Dry Eye Disease:
various complaints of eye irritation
increased blood flow on the ocular surface that leads to reddening
often blurred vision with or without wet eyes
sticky eyelids due to increased production of mucus and other secretum
irritation of nerve fibers is triggered by surface damage
Nerve fibers are particularly numerous on the surface of the eye, which is why it is so sensitive to touch, foreign bodies and dryness.
triggers irritation of the nerve fibers and thus induces a new blink or increased tear flow.
repeated irritation leads to symptoms of eye irritation that are known to all patients.
chronic irritation can also lead to pain and can possibly develop into a pain syndrome
Inflammatory reactions can make the process worse.
Oil Deficiency as the most common primary cause
According to the current state of scientific knowledge, the vast majority, ie four out of five patients with a dry eye, do not have a primary lack of tear water, as one might suspect, but a causal lack of OIL on the tear film.
Lack of oil is caused by meibomian gland dysfunction (MDD) then leads to increased evaporation with decreasing stability of the tear film ... and usually later lack of water .
Therefore, it does not seem to make much sense to use products that do not contain lipids in most dry eye patients today.
It is also possible to use additions of other substances which replace the action of the lipids, or even only lipids, for example as a liposome spray.
In other words, lipids or other substances with a comparable effect should now be part of a typical tear supplement therapy / tear substitute for the dry eye.
A lack of oil is typically caused by constipation of the meibomian glands in the eyelids
The occurring lack of oil is typically due to a malfunction of the meibomian glands, the meibomian gland dysfunction ( MDD ).
It usually consists of constipation of the many small oil-producing meibomian glands in the eyelids.
A diagnosis of the glands can be used to check whether the meibomian glands are blocked .
Gland obstruction comes from oil and dander
The glandular openings on the edge of the lid are blocked by thickened oil and increased cornification and desquamation of the glandular tissue and skin on the edge of the lid.
This is the most common cause of Dry Eyes.
The thickened oil is no longer clear and fluid, but becomes whitish to yellowish and viscous. The thicker it gets, the harder it is to squeeze out.
Oil and dander can form a plug in the gland opening on the edge of the lid.
Thickened secretion builds up in the glands and becomes increasingly viscous and harder.
Therapy : Therefore, a frequently performed treatment consists in heating the eyelids with the glands in them sufficiently to liquefy the fat and to be able to massage it out.
Obstruction of the meibomian glands leads to oil deficiency and unnoticed glandular destruction
2 Causes
The meibomian gland dysfunction (MDD) with constipation of the glands typically has two causes :
Thickening of the oil in the duct system in the glands
Horny gland opening
=> Both together lead to the blockage of the gland opening ( picture ).
2 Consequences:
The obstruction of the Meibominan glands has 2 main Consequences (please see Image):
Dry Eyes because of the oil deficiency on the tear film and increase evaporation of the tear water, termed as an ´Evaporative Dry Eye´)
progressive self-destruction of the gland tissue inside the eyelids due to the increased pressure inside the blocked glands
Therapy:
Therefore it is important
to treat not only the resulting oil deficiency in Dry Eye Disease, e.g. by Tear Supplements
but also to address the causative gland blockade , e.g. by Physical EyeLid Therapie with warming, gland expression and EyeLid Hygiene
Risk Factors
Various influencing factors damage the tear film
The production and maintenance of the tear film is very complex in our dry environment, and it is therefore very susceptible to failure .
The tear film is dependent on many and very different influencing factors that can change the tear film in any way positively or negatively.
All negative factors are risk factors - sooner or later, and especially if they become chronic, they can lead to a dry eye.
The large number of risk factors, which may seem unrelated at first glance, often give the impression that the dry eye is a " tricky disease " - although the connections are actually quite simple.
External risk factors
Environmental Factors
In everyday life, external environmental factors are particularly important as risk factors. These are all influences that can disturb and damage the finished tear film on the eyes, e.g. smoke, dust, preservatives in eye drops, contact lenses.
Drying out environmental influences such as warm and dry air, blowers in cars or in air conditioning systems, etc. are particularly common here . Therefore, a dry eye generally occurs more frequently in dry or moving room air from air conditioning systems and during the heating season in winter. Here simple ' home remedies ' can already prevent and improve.
Eye Drops
Drugs that reach the eye surface from outside as eye drops are, of course, also external risk factors. Depending on the active ingredient used, they can, under certain circumstances, damage the tissue of the eye surface and contribute to dry eyes, especially if the eye drops are applied permanently.
This is particularly important if eye drops contain preservatives. Preservatives are usually relatively aggressive substances which kill microbes and thus should keep the eye drops germ-free. However, they can also attack the cells of the ocular surface and thus damage the tissue on the surface of the eye and thus contribute to dry eyes. The more often such eye drops are used and the more aggressive a preservative they contain, the greater the risk of possible damage.
For more information, please consult your eye doctor.
Internal risk factors
Internal risk factors arise from malfunctions in our internal regulatory systems (nervous system, hormone system, immune system) and from systemic diseases that have a negative impact on eye health and tears.
increased age and chronic diseases
The normal aging processes in the body also affect the functionality of the eye.
This leads to, for example
decreased watery tear production
increased cornification of the skin on the edge of the eyelid with an increased tendency to blockage of the meibomian glands
Increased tendency to change the shape of the eyelids with disturbance of the formation of a stable tear film
Increased tendency to chronic systemic diseases , such as cardiovascular diseases (e.g. high blood pressure), metabolic diseases (e.g. diabetes mell., thyroid disorders), chronic inflammation (e.g. rheumatic diseases).
Even drugs that chronic diseases for treatment are used, may have a negative impact on the health of the eye and convey a dry eye.
Hormones are another important risk factor and this also affects the changes in hormones with increasing age.
The sex hormones are of particular importance , among other things because they act on the glandular tissues. Men and women have both male sex hormones (androgens) and female sex hormones (estrogens, progestogens) - but in different amounts.
In general, and very much simplified, male sex hormones are considered to be rather beneficial for the glands, tear system and surface of the eyes, while female sex hormones are considered to be rather negative. However, this also depends on age and many other factors.
The important influence of sex hormones explains why the dry eye generally occurs more often in women and increases with age in both sexes. In menopause and menopause, the frequency of dry eye increases in women - according to studies, hormone replacement therapy leads to a further increase.
... some BASIC ideas for THERAPY
What can I do ? … as a therapy for dry eye disease ?
Different inter-related factors contribute to ocular surface disease including the dry eye. These can be approached and improved by different therapy approaches:
Typically there is a deficiency of the Tear Film based on a qualitative or quantitative lack of tear components. Tear Supplementation, i.e. the addition of missing tear components, is thus the most frequently used therapy option.
The main reason for dry eye disease is a lack of oil due to obstruction of the Meibomian glands. This allows a semi-causative therapy to improve the gland function. A ´physical lid therapy´ with heat and lid massage can be performed at home by the patients.
All types of dry eye disease and chronic eyelid inflammation (blepharitis) are related to the accumulation and incrustation of debris on the lid margin that leads to worsening of the condition. Therefore specific lid hygiene to clean the eyelids and a general eyelid care is useful to promote the health of the ocular surface and thus to improve dry eye disease.
TEAR SUPPLEMENTS are a cornerstone of Dry Dye therapy
In dry eye disease there is typically a deficiency of the tear film based on a deficiency in the amount or quality of tear components.
Therefore, the most common therapy is tear supplementation, i.e. the addition of (missing or insufficient) tear components.
This is often referred to as 'tear replacement' or ´artificial tears´. Unfortunately, it has not been possible at present, and for the foreseeable future, to completely replace the natural tears. The term tear supplements thus appears to be most appropriate.
An almost unmanageable number of different tear supplements is available. These are mainly eye drops, that are based on aqueous solutions and that can contain different additional active ingredients. Most of the tear supplements are available as over-the-counter products without prescription.
Physical LID MARGIN THERAPY is a basic therapy for Meibomian Gland Dysfunction (MGD)
It can improve oil deficiency and potential gland damage by reactivating the meibomian oil glands inside the eyelids
The concept of ´physical therapy´ is based on simple but effective physical techniques for the treatment of the eyelids and the meibomian glands. Heating and humidification, massage and squeezing as well as subsequent intense cleaning of the lid margin is performed.
Before any manipulation of the eyelid and eye, it is of course important to consult an ophthalmologist beforehand in order to get a qualified diagnosis and appropriate therapy suggestions to avoid injuries to the eyelid and eye ! It is also important to have the potential progress or failure of therapy followed by the eye doctor !
Dry eye disease is a chronic illness, that has typically developed over a period of years or often decades and thus it is often necessary to perform an equally consistent permanent i.e. ´chronic´ treatment. Long-term physical therapy is therefore typically necessary about once or twice daily.
The Methods of Physical Therapy can be applied in different ways (=> HERE is more information):
as BASIC Therapy at home - this will be described here below
as APPARATIVE Device-Based Therapy - this is performed in the eye doctor´s office. The application of specialized equipment is typically more effective and results in a quicker improvement of symptoms. In addition, specialized devices offer novel therapy options that are not available at home.
=> here is an Overview of all methods for the therapy of the eyelids and Meibomian glands.
Physical therapy consists of 3 steps:
1. Warming of the eyelids
if possible with moist heat for at least 10 minutes
to achieve a temperature of approx. 40 ° C inside the eyelid, i.e. also in the Meibom oil glands
serves to re-liquefy the changed and hardened oil in the meibomian glands.
according to studies, in order to reach a temperature of 40°C in the eyelid, a warm, moist compress / clean washcloth (with a temperature of approx. 45 ° C) must be used for approx. 10 minutes; (please see animated figure)
as the temperature cools down quickly, the compress/ rag must be renewed/ reheated approximately every 2 minutes
The moisture softens encrustations at the gland openings and on the edge of the lid
Commercially available Gel Masks or even electrically heated and moistened Goggles can make the laborious physical EyeLid Therapy können significantly easier.
2. Subsequent massage of the eyelids to squeeze and empty the glands
when the inspissated oil in the meibomian glands is warmed up enough, it becomes more fluid again
by gently massaging the eyelids, it can then be squeezed out of the glands
this must be done towards the open edge of the eyelid (´eyelid margin´ - see animated figure) - so:
down the upper eyelid and
upwards on the lower eyelid
in any case, as already mentioned, a chronic illness like dry eye disease with Meibominan gland dysfunction, also requires chronic therapy in order to achieve noticeable improvements.
Therefore, even a properly performed gentle eyelid massage does not necessarily always lead to visible expressed inspissated Meibom oil on the lid margin.
Still, a consistently performed physical therapy typically results in a constant improvement of the condition … constant dripping wears the stone !
... if the glandular squeezing does not achieve a sufficient improvement of gland function despite long (over months) regular and careful application, then there are further specialized procedures and devices for the therapy of Meibom gland disorders (MDD) and eyelid inflammation (Blepharitis) in the ophthalmologist's practice.
3. Eyelid margin hygiene at the end
Finally, the eyelid should be cleaned together with the eyelashes:
of the squeezed oil
of bacteria that multiply in the oil residues
of hardened lipid deposits and skin cornification on the edge of the eyelid
Cleaning consists of a mild (soap-free ) 'scrubbing' of the edge of the eyelid with a cotton swab or facial tissue to remove deposits that can promote inflammatory events:
if the deposits are more liquid-oily, a dry cotton swab can often do a good job
if the deposits are rather dry and crusted, a damp cotton swab is usually more suitable
There are also commercially available cleaning sets with solutions, typically oil-based so as not to damage the tear film lipids. Such sets already contain all the necessary things and can thus make physical therapy considerably easier. Pre-prepared sterile cleaning pads are available for daily lidcare.
In case of a chronic therapy-resistant chronic eyelid inflammation (blepharitis), an increased infestation with normal Demodex hair-mites may be considered, which are sensitive to a therapy with tea tree oil products.
Overview of the options of physical therapy
The physical therapy measures shown here have the advantage that they can usually be carried out by the patient himself in his home environment. This is the BASIC therapy for meibomian gland dysfunction (MDD) and chronic eyelid inflammation (blepharitis).
=> here you will find more information about BASIC Therapy at home
A disadvantage may seem to be that this has to be done permanently and regularly, preferably twice a day, in order to achieve a noticeable positive effect - similar to brushing your teeth - but requires a little more time.
If the basic therapy of the eyelids at home does not achieve a sufficient improvement in spite of a longer period of regular practice, there are other specialized procedures and devices for the APPARATIVE therapy of meibomian gland dysfunction (MDD) and chronic eyelid inflammation (blepharitis) in the ophthalmologist's practice.
=> here you will find more information about APPARATIVE device therapy in the medical practicebut ... the effort is worth it, because a 'happy' eyelid typically ensures a happy patient!
... or to put it in Roman form: ´ palpebra sana in corpore sano ´ - unconfirmed quotation from the famous Roman doctor Clarissimus GALEN ;-)
QUICK GLIMPSE on …
Contact lenses
Contact lenses are a fantastic optical tool with a close relationship to the surface of the eye and also to the dry eye
Contact lenses are a fantastic optical aid, with some clear optical advantages over glasses.
At the same time, they allow greater " freedom " for leisure activities, sports and social appointments.
Dimensionally stable contact lenses (illustration) are relatively small and only sit on the cornea . This type of lens is particularly stable and has high optical quality. Modern lenses also have high oxygen permeability.
In the past, these lenses were made of a different material (plexiglass) and were therefore called "hard" contact lenses.
In addition to being worn normally, dimensionally stable contact lenses are also suitable for optically correcting an irregular corneal surface ( astigmatism - often called astigmatism ). Strong astigmatism can often not be completely compensated for with glasses.
Contact lenses sit in the 'middle' of the eye surface
As their name suggests, contact lenses are in direct contact with the surface of the eye.
Contact lenses are located right in the middle of the functional unit of the surface of the eye - on the eyeball and behind the lids in the conjunctival sac .
This means that they have a possible influence on all tissues and on the tear film . With every blink, for example, the back edge of the upper eyelid (illustration) must slide over the edge of the contact lens when the lid is closed. This is a common area for irritating irritation.
Contact lenses therefore have a somewhat ambiguous effect on the eye - with advantages and disadvantages.
' Soft' contact lenses (Figure), also called hydrogel lenses, are the most common type of contact lenses. This is probably due to the fact that it takes little or no time to get used to the lenses until they can be worn without discomfort and irritation.
Soft lenses are larger than dimensionally stable contact lenses and extend beyond the cornea to the conjunctiva.
Contact lenses float in the tear film on the eye ... and have increased demands on the tear film
In principle, contact lenses place higher demands on the quantity and quality of the tear film .
It is possible that someone with no signs of dryness will develop dry eye symptoms after inserting a soft hydrogel contact lens . This may be due to the fact that there was a borderline normal tear film that is no longer sufficient for a contact lens.
A typical side effect of wearing contact lenses is therefore the appearance of symptoms of dry eyes or even the development of a dry eye .
If there is already a lack of tears, contact lenses should not be worn. Permanent wetting with tear substitutes / artificial tears is also not a recommended permanent solution.
The only exception is wearing therapeutic scleral contact lenses.
Scleral contact lenses can be used to treat very severe dry eye
Although the widespread soft contact lenses can cause or worsen a dry eye, another special type of contact lens (scleral lens) can be used as a therapeutic aid in patients with severe dry eye .
Scleral contact lenses are very large and dimensionally stable. They cover the cornea with a teardrop lake and extend far beyond the conjunctiva. Underneath is the hard eye wall ( sclera ). The surface of the eyes is constantly bathed in a lacrimal lake and a heavy dry eye can be kept permanently moist.
Because scleral contact lenses span the cornea, they can also compensate for very severe irregularities in the cornea, for example when the keratoconus is disturbed .
These large lenses require a very special adjustment by an experienced contact lens specialist. It becomes clear that contact lenses are a medical device (medical device) with a direct impact on the eye , which requires careful selection, adjustment and follow-up .
The adaptation of a contact lens determines its influence on the surface of the eye:
An exact adjustment is necessary for contact lenses!
( 1 ) In order to keep possible damage to the eye to a minimum, contact lenses must always be precisely adjusted by a specialist .
If the adjustment is too flat, the contact lens is mainly on the middle of the cornea.
If the adjustment is too steep, the edge of the contact lens will rub against the conjunctiva of the eyeball.
With any type of adjustment, rubbing the edge of the contact lens on the back edge of the eyelid is inevitable due to the movement of the upper eyelid during frequent blinking (approx. 5-10 times per minute)
A well-adapted contact lens can also change when worn on the eye as well as during cleaning and storage. In addition, minor damage to the lens can occur during handling. This can lead to a changed fit on the eye and thus possibly to increased friction.
( 2 ) Contact lenses should therefore be checked by a specialist at regular intervals after the adjustment .
Contact lenses can have a negative impact on the fine structure of the surface of the eye
Although the usual adaptation principles typically aim to avoid excessive mechanical contact with the surface of the eye, contact lenses are inevitably in contact with the surface of the eye, just as their name suggests.
Contact lenses can therefore have varying degrees of mechanical and chemical influence on the surface of the eye.
This primarily concerns the interaction of the contact lens with the very sensitive central cornea and the similarly sensitive posterior edge of the lid .
The conjunctiva on the eyeball and on the back of the eyelids is less sensitive, but it is also in contact with the contact lens and therefore also exposed to a possible negative influence.
Chronic mechanical irritation of the conjunctiva can lead to squamous metaplasia
The conjunctiva / conjunctiva of the eyeball has been shown to change when wearing contact lenses . This happens in the area where the edge of the contact lens rests and rubs with every eye movement.
The epithelial cells change and the mucus cells that moisturize the surface become fewer and disappear, at least in the area in which the contact lens rubs.
The normal cubic cells of the conjunctiva are transformed into flat cells and this forms a squamous epithelium - a different type of tissue than is normally present here.
This is called squamous metaplasia (see figure). This disrupts the important wetting of the eye surface and promotes the formation or worsening of a dry eye.
Hygiene - a crucial factor when wearing contact lenses
With contact lenses there have been enormous improvements in the material quality and in the shape of the lenses in recent decades. This has led to a reduction in the frequency and severity of contact lens side effects.
However, hygiene is still a very important issue , above all ... but not only ... for inexperienced contact lens wearers.
Inadequate hygiene can lead to serious eye infections , which can endanger vision and, without immediate adequate therapy, can even lead to eye loss.
Dangerous infectious agents (bacteria, amoeba and also fungi etc.) are typically introduced through the handling of the contact lenses, either by the wearer or, for example, by contaminated water.
Therefore, contact lenses should never be treated with tap water and should not be worn while bathing or showering .
Microbes multiply in the contact lens containers or in hard-to-remove deposits (biofilm) on the contact lenses themselves.
The emergence of infections is further promoted by constant micro inevitable injuries, which by normal contact lens wear arise. These small injuries open an entrance gate for the microorganisms through the normally practically impenetrable dense surface of the eye .
Microbes are hidden in the biofilm
Bacteria and other pathogens produce a material called biofilm around them on the contact lens and in the storage container .
Biofilm is a protective layer for the bacteria that is very difficult to remove and requires thorough mechanical cleaning, for example with cleaning solution and rubbing with your fingers . In biofilm, they are not safely destroyed by disinfectant solutions either.
Contact lenses must be cleaned and disinfected thoroughly
For a thorough and safe cleaning of contact lenses and storage containers , the following is required:
(Fig. 2) mechanical cleaning
to remove
Deposits from the tear film (oil, protein, mucilage, salts)
bacterial biofilms in which bacteria hide and protect
(Fig. 3) a subsequent disinfection - bubbling peroxide solutions, for example, are proven overnight.
to kill microbes that could lead to infection
after inserting the lenses on the eye, it is very important to let the storage container dry out !
Further information on contact lens hygiene can be found => here
Disposable DAILY contact lenses have many hygienic advantages
Especially inexperienced contact lens carriers have an increased risk of eye infections.
People with a reduced immune system , such as children and the elderly, are also at greater risk from eye infections.
For soft hydrogel contact lenses are daily disposable / one-time contact lenses a good solution.
They are worn for only one day and then disposed of.
The next day, a new sterile packed contact lens is inserted. This can avoid most hygienic problems.
Daily lenses no longer need to be cleaned and stored. By avoiding these critical steps, bacterial growth is in principle greatly reduced.
Daily lenses are relatively more expensive than lenses that are worn longer (over 14 days to 1 month). However, they no longer need to invest in cleaning solutions and do not have to be laboriously cleaned daily. Both reduce the effort with this type of lens.
In terms of hygiene, daily lenses have a clear advantage and the infection rate is lowest with this type of lens.
=> HERE you can find MORE information about contact lenses
OVERVIEW

Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT ]
OVERVIEW
The ´doctor´s page´ will deal with:
PHYSIOLOGY surface of the eye
PATHOPHYSIOLOGY in the dry eye
Typical SYMPTOMS
Important FINDINGS
Pioneering DIAGNOSTIC TESTS
SEVERITY division
THERAPY Step Plan
Please choose a TOPIC of your interest by clicking on an image - or just follow the presentation on this page ... which is perhaps the most informative
Basic PHYSIOLOGY
of the ocular surface
The surface of the eye is a permanently moist tissue
The OCULAR SURFACE is the permanently moist mucosal tissue on the front of the eyeball.
The tear glands and the draining tear ducts form the mucosal adnexa and belong to the surface of the eye.
The indispensable moisturizing, and thus eye health, is maintained by a few basic functional complexes.
Basic FUNCTIONAL COMPLEXES
2 essential functional complexes ensure the moisture of the ocular surface as a basic requirement for its health:
Tear production
Tear distribution into the tear film
The eyelids spread the tears within the interpalpebral cleft into the extremely important thin tear film
Only the tear film can secure the moisture on the eye even when the lids are open - and at the same time it improves the refraction of light for optimal visual acuity.
A new vision of the ocular surface
The observation of the ocular surface via its functional complexes, which are important for intact function and thus also for the maintenance of structural integrity, results in a new image of the ocular surface.
The schematic representation of the functional complexes in their interaction as pictograms is intuitively understandable.
This new image leads to a holistic and dynamic concept of the ocular surface and from there to a holistic dynamic concept of dry eye disease.
The intact cell surface with its goblet cell glands is important for the wettability of the ocular surface:
The goblet cell glands (pink in the image) in the conjunctiva produce soluble water-binding mucins to form a mucin-water gel in the tear film
the intact cell surface is an indispensable prerequisite for eye health.
numerous micro-processes (microvilli and microplicae) and the integral mucins of the glycocalyx in their cell membrane allow the aqueous tears to adhere
= these structures can only be seen in the electron microscope .
PATHOPHYSIOLOGY of dry eye disease
Various factors are involved in the pathophysiology of dry eye disease and are explained individually below. Finally there is a summary.
Triggering CAUSAL FACTORS
Triggering causal factors for dry eye are disorders that lead to the formation of an insufficient tear film. Above all, these are:
Deficiency of tear production
quantitative or qualitative
by the various glands of the eye
the dysfunction of the meibomian glands is the main cause of a dry eye, according to current knowledge.
including the intact cell surface with goblet cell glands and mucin formation.
Deficiency of tear film distribution/ spreading
due to any disorder of the eyelids themselves or of their regular blinking movement, e.g. by:
Neural regulation disorders
Shape and position of the eyelids
is typically disturbed in the normal aging processes, when the eyelid tension decreases or the eyelid shape is twisted by a scarning condition.
Primary PATHOLOGY
The two primary pathologies in dry eye are
Tears film deficiency and
Tissue damage
Both pathologies are called "primary" because both of them can occur first and then induce the other one.
A typical consequence of the tear film disorder is damage to the sensitive cell surface .
this is clinically detectable as vital staining surface speckle (keratitis superficialis punctata, KSP), usually by using fluorescein.
Later there can be extensive damage with a degenerative remodeling of the tissue
Rarely, the tissue of the surface of the eye is damaged first, which can later lead to disorders of tear adhesion and thus moistening.
Secondary Pathogenetic Factors … occur as consequences of tear film deficiency and tissue damage
Subsequent secondary pathogenetic factors develop in both primary pathologies of the dry eye (tear film deficiency and tissue damage):
they are interlinked and
drive the disease process forward in cascades
the secondary factors can be collected as clinical findings
a severity stage of the dry eye can be classified based on these findings
TEAR FILM deficiency
With tear film deficiency, it is not always easy to assign the secondary pathogenetic factors exactly to the deficit of a certain tear component, ie a lack of
or to blinking disorders
According to the current understanding, in addition to a generally possible decrease of the visual acuity, the following assignment of symptoms can be carried out:
Aqueous tear deficiency ... leads to
Wetting problems with the development of 'dry spots' in the tear film
Increased mechanical friction .
due to reduced lubrication between eyelids and globe
is exacerbated by wearing contact lenses, especially if there is a lack of aqueous tears.
Chronic mechanical irritation
leads to tissue remodeling and is an inflammatory stimulus
Lipid / oil deficiency ... leads to
Tear film instability with short tear film breakup time (TAZ / BUT) followed by
faster evaporation of the tear water (hyper-evaporation) with subsequent
so-called "Evaporative Dry Eye"
increased osmolarity (hyperosmolarity) of the remaining tear film
when the tear water evaporates, the dissolved substances (proteins, salts) remain and their concentration in the remaining tears increases (please see animated figure).
this is also an inflammatory stimulus .
Blinking disorder => disruption of tear film spreading ... leads to
Tear fluid alone is not sufficient for a tear film because only the normal and sufficiently frequent blinking movement of the eyelids creates the necessary film from the tear fluid.
A disorder of the eyelids themselves or the normal blinking of the eyes therefore causes a tear film disorder or can contribute to it.
Consequences are, e.g.
disruption of tear film spread
increased eyelid friction on the eyeball
chronic mechanical irritation
this is an inflammatory stimulus
Mucin deficiency ... leads to
Wetting problems
Unstable tear film, short tear film break-up time (BUT)
possibly also responsible for patients with very short BUT drye eye
'dry spots' in the tear film
increased mechanical friction and leads to chronic mechanical irritation of the epithelial cells
=> this is an inflammatory stimulus
Mucin deficiency occurs when the fine structure of the cellular surface, including the membrane-bound mucins on the microvilli and the soluble mucins of the goblet cells are damaged by:
topical damage (mechanical or chemical) in the case of disorders of the tear film - this is the typical course in the dry eye ... or by ...
Systemic damage, for example due to severe vitamin A deficiency or chronic inflammatory diseases that also involve the surface of the eye.
SURFACE TISSUE DAMAGE occurs as a consequence of tear film deficiency
The main pathogenetic factors of tear film disturbance (hyper-osmolarity and chronic mechanical irritation) lead to chronic damage to the tissue surface .
Chronic damage to the cellular surface induces
chronic inflammation, which ultimately leads to
degenerative tissue remodeling with
increasing loss of function.
Degenerative Tissue Remodeling and Loss of Function occurs in chronic tissue wounding
The chronic surface damage in dry eye affects first the epithelium, and has several downstream consequences, that act as secondary pathogenetic factors in the disease process.
These are interrelated, mutually reinforce each other and drive the disease in a pathological cascade if they are not treated by timely and effective therapy:
Damage to the fine surface structure :
the number of goblet cells on the conjunctiva decreases and squamous metaplasia develops.
this reduces the ability to bind the aqueous tears to the surface ('wettability') .
=> Reinforcement of tissue damage to the surface of the cornea and the conjunctiva (image).
Activation of cells of the surface epithelium .
=> creates an inflammation.
the cells form inflammation mediators (cytokines and chemokines) such as interferon gamma (IFN-g), tumor necrosis factor alpha (TNF). These expand the inflammation and make it worse.
Abnormal cell differentiation and angiogenesis
Chronic inflammation
Chronic friction and increased osmolarity of the tear film are inflammatory stimuli.
Since Risk Factors for a Dry Eye typically occur chronically the resulting tissue irritation cannot be eliminated by the inflammatory reaction.
Therefore, also the inflammatory tissue response becomes chronic and a progression occurs from subclinical to clinical inflammation
The inflammatory response is a response of the cells to harmful stimuli /adverse events/ noxae that threaten their integrity and function.
Inflammation is a very old protective mechanism for practically all cells and tissues of the body, especially against infections with bacteria and other microorganisms.
Typical 'side effects' of inflammatory reactions are further damage to the body's own tissue. This is accepted by the tissue as 'collateral damage' with the intention of eliminating the noxious substances as effectively as possible. In case of infections, inflammation is often effective against the pathogens. With chronic (mechanical and chemical) trauma in dry eye, this cannot work. The result is a senseless tissue damage that continues.
Immunomodulated inflammation
Chronic inflammation disturbs the normal immune tolerance of the body and therefore an immune-modulated inflammation can arise, which is modulated by T-lymphocytes.
This type of inflammation is very powerful and can lead to severe chronic inflammation with significant damage.
This finding of immune modulated inflammation in Dry Eye Disease is the basis for the use of anti-inflammatory medication, for example with lymphocyte inhibitors (such as the calcineurin inhibitor cyclosporin A, CsA) in the dry eye
The inflammatory reactions that occur drive self-reinforcing control loops of the disease exacerbation (Vicious Circles) and are an important reinforcement mechanism of the dry eye.
SYNOPSIS of the Pathophysiology in Dry Eye Disease
In the synopsis (see animation) the basic causal factors lead :
Disorder of the glandular tissue and / or
Eyelid disorder
to a disturbance of the tear film and thus the constant moistening. This triggers the two primary pathologies :
Tear film deficiency and
Tissue damage
The primary pathologies are governed and promoted by cascades of secondary pathogenetic factors . These can be collected as clinical findings and serve
Diagnostics and
staging
Risk factors
Various influencing factors inside and outside of the body can have a negative effect on the basic functional complexes of the surface of the eye or on the tear film. Therefore they represent risk factors and can promote the development and worsening of a dry eye.
The influence of various risk factors must be considered when assessing the development of the disease. This can help to identify the appropriate therapy options for an individual patient.
Important risk factors
Disorders of the body's regulatory systems that control the surface of the eye (such as the nervous , endocrine, and immune systems )
Internal risk factors, such as age, gender, chronic illnesses, medication or drinking amount and diet, can have a negative impact on the tissues of the ocular surface.
these include, for example, decreasing aqueous tear secretion with increasing age, increasing cornification at the edge of the eyelid, increasing tendency to eyelid deformities (entropion, ectropion), often decreasing drinking volume and a poor diet, etc.
External risk factors in the environment dry out the tear fluid and the tear film. These include, for example, drafts, dryness, dusts in the air, rare blinking or wearing contact lenses. An accumulation of such risk factors occurs in computer work environments in the office. In this context, the dry eye is known as “office eye”.
Iatrogenic dry eye
Various medications can favor dry eyes
Often underestimated internal risk factors for a dry eye are, in addition to chronic systemic diseases, various medications for the therapy of such disease.
Drugs are of negative influence for the dry eye if they change the inner milieu of the body in such a way that the production of components of the tears is disturbed or if the surface of the eye is directly changed.
Dry eye conditions that are negatively influenced by medical treatments of any kind are termed ´ Iatrogenic dry eye ´. In the current TFOS DEWS II Report (2017) a special chapter was devoted to the iatrogenic dry eye. Further details can be found in a current German-language review on the dry eye.
Many classes of medication have long been known to carry dry eyes. These include, for example
Antihypertensive drugs, such as beta blockers
some anti-cholinergics like
Anti-histamines
various antiarrhythmics
various bronchodilatants
various anti-depressants, sedatives
some anti-Parkinson medication
some pain relievers (canabinoids, opioids)
Hormones (eg estrogens, anti-androgens)
If it is suspected that a medication could promote or worsen a dry eye, the necessary desired effect must always be weighed against possible undesirable effects in order not to endanger health. Medications prescribed by a doctor should not be discontinued on your own !
Preservatives in eye drops can damage the cell surface
Preservatives in eye drops are among the external risk factors. They are still in many eye drops and can cause direct damage to the surface of the eye.
Preservatives in eye drops are substances that effectively kill germs of different kinds … but, as a side-effect, they can often also effectively kill the body’s own cells.
Especially if eye drops have to be administered chronically and frequently (such as tear substitutes or anti-glaucomatous eye drops), the preservatives contained can damage the tissue and thus the stability of the tear film.
However, a possible negative influence depends on the specific preservative and the dosage.
If it is suspected that a medication may promote or worsen a dry eye, the necessary desired effect must always be weighed against possible undesirable effects in order not to endanger health. Medications prescribed by a doctor should not be discontinued on your own!
Unfortunately, the Dry Eye tends to worsen without timely and effective therapy
The complex pathological changes in dry eye have a tendency to influence each other negatively and thereby reinforce the disease process. This is also called self-reinforcing vicious circles.
It leads to a progression in the severity of the disease if timely and effective therapy is not carried out.
The two primary dry eye pathologies, as explained above,
tear film deficiency and
tissue damage
=> both of these damage the glands of the eye (tear glands and meibomian glands) as well as the goblet cell glands in the conjunctiva and thus the mucin production and wettability of the surface.
Ocular surface damage induces
disorder of the sensory nerves on the surface with subsequent
disruption of neural autoregulation of secretion and blinking
disorder of the eyelid margin due to chronic blepharitis
=> these secondary pathogenetic factors of gland damage drive large ´ pathological carousels ´, which then intensify the primary pathologies of tear film disorder and tissue damage.
Many self-reinforcing loops that affect each other come together in the pathophysiology of dry eye. This creates a rather complex interaction of various disease factors (please see figure). This explains why dry eye therapy is still a challenge for both patients and doctors.
Self-reinforcing Vicious Circles of disease aggravation - numerous and different
Contrary to the assumption that in the pathophysiology of the dry eye ´ there is only one ´self-reinforcing vicious circle´ for aggravation of the disease, there are in fact many and different ones that are inter-related.
Against the assumption of a single self-reinforcing control loop, there is also the argument that a therapy could then be applied to any pathophysiological factor and would still always be successful. This is not confirmed by decades of experience in dry eye therapy.
The vicious circles are partially reinforced by inflammatory mechanisms, some of them, however, also work without inflammation.
A typical feature of an advanced stage of dry eye disease is the development of numerous different Vicious Circles, for example:
A lack of tears leads to tissue damage of the surface - and this in turn worsens the wetting and increases the triggering lack of tears.
Surface damage induces inflammatory reactions and this can intensify the triggering damage
Surface damage disrupts the sensory innervation from the surface of the eye. This disrupts neural autoregulation for secretion, leads to a lack of tears and thus increases the triggering surface damage.
etc.
The progression of the disease is even accelerated by immune-modulated inflammatory reactions. This can result in:
Degenerative remodeling of the tissue and
Loss of function of the surface of the eye
Typical SYMPTOMS
Damage to the dry eye leads to some typical SYMPTOMS
A detailed description of the symptoms can be found in the chapter “More information”
In summary, typical dry eye symptoms are based on dryness, irritation / irritation, and pain .
Initially, especially in the elderly, eye irritation may occasionally lead to increased lacrimation / lacrimation and wet eye .
Furthermore, the optical consequences of the disturbance of the normally uniform tear film are noticed as: deterioration of visual acuity / blurred vision / unstable vision.
It is typical of the dry eye that the subjective symptoms do not always exactly match the clinical findings .
TYPICAL FINDINGS
=> You can find a short overview of typical conditions with dry eyes => HERE
Diagnostic tests
=> You can find a brief overview of pioneering DIAGNOSTIC TESTS in the dry eye => HERE
SEVERITY
For the dry eye, a rather general division into 4 levels of severity has prevailed, ranging from easy to moderate and difficult to very difficult . Ultimately, the decisive factor is the extent of the surface damage that occurs in vital staining.
However, there is currently no generally accepted definition for the exact classification of the degrees of severity according to clinical findings.
For the meibomian gland dysfunction there is also a blockage of the glands, which ( still ) runs without symptoms and therefore has the severity level "0".
In contrast, a dry eye is by definition always symptomatic and the severity classification therefore begins with “° 1” / “easy”.
The consensus reports of the international “Tear Film and Ocular Surface” (TFOS, www.tearfilm.org ) have a certain level of acceptance.
In the TFOS “Dry Eye Workshop Report” (DEWS) from 2007, an exact severity classification was given based on numerous criteria
In the TFOS “Dry Eye Workshop Report II” (DEWS II) from 2017, such a small-scale definition receded in favor of more general considerations. There are some important parameters classified in stages, such as severity of the evaporative disorder, severity of tears and surface damage.
There is a severity classification according to the height of the tear meniscus is suggested:
0.2mm: mild
0.1 mm: moderate
0 mm: heavy
Evidence of a dry eye
No single criterion is certainly sufficient for reliable grading of the dry eye .
Both with the tear film parameters , which can often be quantitatively evaluated today ( lipid layer thickness , instability / BUT , tear meniscus , osmolarity ) as well as with the gland parameters ( aqueous secretion / Schirmer-1 test , oil secretion / diagnostic expression , meibography ) individual findings can not provide reliable evidence of dry eye.
A lack of, for example, watery tear secretion, even if it is very pronounced (less than 1 mm), cannot be reliably demonstrated by a severe dry eye. A practically dry umbrella test strip should perhaps first lead to the suspicion that this was carried out incorrectly, eg if the strip did not reach far enough into the lower fornix. Isolated deviations in the thickness of the lipid layer on the tear film or in the osmolarity are also an indication but not a reliable proof of a dry eye.
Of course, a consistent moderate to severe deficiency of various factors such as watery tear secretion, oil production, tear meniscus and tear stability makes dry eyes increasingly likely.
Practical clinical severity classification
The most reliable evidence of an effectively “dry” eye , ie symptomatic surface damage with tear film disorder, is the tissue damage that has already occurred:
this is typically caused by a previous chronic tear film disorder.
Occasionally there may also be primary chronic tissue damage , which inevitably leads to a tear film disorder.
Tissue damage is typically demonstrated as vital staining in the sense of superficial punctate keratitis (KSP).
The extent of the vital staining also gives a reliable indication of the severity of the dry eye .
If the vital staining is evaluated according to the established Oxford scheme , then there is a division into the 4 levels mentioned, from easy to moderate and difficult to very difficult .
There is an advanced level 5 for even more difficult findings, but this is of no essential importance for practical clinical work.
THERAPY
=> You can find a short overview of the established step therapy for dry eye => HERE
=> You can find basic considerations for various therapy options => HERE
Continue to chapter
Deeper insight
Deeper
INSIGHT

Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT ]
DEEPER
INSIGHT
The ´SCIENTIST´s Page´ is open to those with deeper interest
... in the OCULAR SURFACE and DRY EYE Disease
Choose a CHAPTER of your interest - or just follow the illustration ... which is perhaps the most informative
THE EYE SURFACE
The surface of the eyes must be constantly moist to remain healthy and to achieve perfect visual acuity
What IS the eye surface?
=> The moist mucous membrane tissue on the front of the eye!
The OCULAR SURFACE is the moist mucous membrane tissue on the front of the eyeball.
In addition to the visible cornea and conjunctiva, which are bathed in tears, the surface of the eye consists of organs hidden under the skin: from the attached lacrimal gland for the production of new tears to the lacrimal drainage channels for the removal of the ' used ' tears into the nose. The tears enter the drainage system through the lacrimal puncta at the nasal side of upper and lower eyelids.
In this drawing, the depth of is conjunctival and the thickness of the tear film is exaggerated, so you can see them - in fact, the eyelids are literally right on the eyeball, the conjunctival sac forms only a wet gap, and the tear film is extremely thin.
The CONJUNCTIVA is a support tissue of the cornea, which contributes significantly to the health of the cornea and the whole eye.
It covers the front of the eyeball and the back of the eyelids by forming the conjunctival sac. The conjunctiva therefore connects the surfaces of the eyeball and the eyelids.
The conjunctival sac is only open to the outside world in the area of the open eyelids, i.e. the interpalpebral fissure. There, the tissue must be covered with a thin film of tears - the tear film that keeps the sensitive cell surfaces always moist, even when the eye is open.
Why does the surface of the eye have to be moist ?
=> To maintain their health and integrity for the transparency of the cornea !
Only a MOIST cornea is TRANSPARENT
The MOISTURE surface of the eye is needed to the cornea / cornea TRANSPARENT keep
The surface of the eye is a moist mucous membrane to keep the cornea / cornea transparent.
The surface of the eyes must be kept permanently moist - always and everywhere - in order to remain intact and healthy and is therefore constantly bathed in the tear fluid.
TEARS are the medium for the moisture at the ocular surface
The continuous flow of tears over the surface of the eye , which is of the utmost importance for your health, goes (from left to right in the illustration): (1) from the main production site in the lacrimal gland via (2) the visible cornea / cornea and conjunctiva / conjunctiva that must be constantly bathed in (3) the lacrimal drainage system , the ' used to derive' tears into the nose.
The tear fluid is formed by the glands at the surface of the eye and after ´use ´ - that is, after bathing the cornea and conjunctiva - the ´used´ tears are transported into the nose by the draining tear ducts.
The continuous new production of tears and the tear flow along the ocular surface is therefore of the greatest importance for your health and for the clarity of the cornea - i.e. for intact Vision.
It is important to remove the 'used' tears in a controlled manner, as there is only space on the surface of the eye for a very small tear volume.
... in fact it is the case that not even a single additional drop of liquid, e.g. from eye drops, has space on the surface of the eye. After applying an eye drop, often most of the liquid runs off again via the edge of the lid.
In contrast to a really 'dry' eye, a temporary increased tear production due to eye irritation can result in episodes of a 'watery wet dry eye'.
Also a disturbed removal of the 'used' tears from the ocular surface, due to obstructed lacrimal puncta, can lead to tears overflowing over the edge of the eyelid.
... we can therefore see that the conditions on the surface of the eye do not differ significantly from our experience in other areas of daily life - both 'too much' and 'too little' can be annoying ;-)
What is the tear film- and what is its function?
=> A multilayered liquid sheat on the eye that ensures moisture and clear vision when the eyelids are open !
Constant moisture for the cornea and conjunctiva in the area of the open eyelid cleft is made possible by a thin layer of tears - the tear film.
It is thin and even enough not to disturb the visual acuity and at the same time sufficiently stable to prevent the tissue from drying out due to evaporation of the tear water in the air atmosphere.
The uniformity of the tear film is of great importance for the perfect visual acuity because the tear film is the first refractive surface of the eye.
Faults and irregularities in the tear film with a lack of tears in dry eye but also with excessive tearing in a wet ´dry eye´ are often first manifested by reduced or fluctuating blurred vision (unstable visual acuity).
The TEAR FILM (left) consists of 3 layers, the components of which are produced by 3 different types of eye glands (right).
The tear film has three layers , which consist of the products of the different glands of the eye surface :
Mucus (mucin ) from individual goblet cells in the conjunctiva forms a thin layer on the cells and only makes the tissue surface wettable for water.
Water , which is the main body of tears, is produced by the lacrimal gland, which is located on the side of the eye socket.
Oil is produced by the meibomian glands in the eyelid and forms a very thin layer on the surface of the tear film - similar to oil on a puddle of water on the roadside. The oil reduces the evaporation of the water and improves the stability of the tear film.
A look into the tear film
A LOOK INTO THE TEAR FILM: The middle main part of the tear film in front of the transparent cornea consists of aqueous liquid. The numerous finger-like extensions (micovilli) of the superficial epithelial cells are visible below - they bind the water to the cell surface. The water is bound by the long sugar chains (here reddish) of mucins. Membrane-bound mucins (glykokalyx) are fixed to the microvilli whereas soluble mucins float in the tear film and transform the water into a low-viscosity water-mucin gel. At the top, the tear film is covered by the very thin layer of oil from the fats of the meibomian glands - this prevents the tear water from evaporating too quickly.
What role does the cell surface of the eye play?
=> Only the intact fine structure of the surface of the eye enables moistening with the watery tears
The intact cell surface is an indispensable prerequisite for moisturizing the eye and thus for eye health.
The cell surface produces mucins that allow the surface to be wetted:
unicellular goblet glands produce soluble mucins. Together with the water from the lacrimal gland, they form a mucin-water gel - this is the main part of the tear film.
all cells form membrane-bound mucins, which are firmly anchored in the cell membrane and bind the watery tears to the cell surface.
In addition, some soluble mucins also come from the lacrimal gland
The cells have numerous fine finger-like extensions that increase their surface area and thus improve water binding.
... accordingly, damage to the cell surface (mechanical or chemical) with destruction of the fine structure leads to disturbances in wetting with tear fluid and to increased dryness and irritation of the eye.
Electron microscopy shows the tiny structures on the surface of the eye
Goblet cells
Goblet cell glands in the conjunctiva produce soluble mucins and release them to the surface in the tear film. They are already visible in the light microscope.
Goblet cells and mucins are marked in pink in the image.
Mikrovilli
The entire cell surface is covered with numerous finger-like protuberances (microvilli and microplicae / microfolds).
these are so small that they can only be clearly recognized by electron microscopy (please see image
Glycocalyx
In the cell membrane of the micro-processes are membrane-bound mucins. They appear as fine tree-like structures (glycocalyx, please see image) and protrude into the aqueous tear film to bind the water.
According to studies, this molecular arrangement is the basis for wettability of the ocular cell surface.
What role do the eyelids play?
=> The eyelids distribute the tears to the important tear FILM in the open eyelid on the surface of the eye!
This schematic simplified animation of the blink movement of the eyelids illustrates the basic function of the eyelids to distribute the tears into a thin film in the area of the eyelid cleft. This allows to keep the tissue of the ocular surface moist even when the lids are open to see. However, actual tear drops (as simplified here) occur in the area of the eyelid cleft only with excessive tear flow.
The eyelids are very important for the health of the eye.
The wiping movement of the upper eyelid when LIDSCHLAG
spread the tears in the thin and even tear film.
it will also squeezed oil from the meibomian glands in the eyelids
and spread the oil on top of the tear film.
The tear film is used to keep the tissue in the open eyelids open and is also the most important surface for correct refraction of the incoming light for perfect visual acuity.
Necessary conditions for a stable tear-film and thus for a healthy eye surface and a perfect visual acuity are sufficient in quantity and quality production of tear fluid by the glands and the formation of a sufficiently stable tear-film through the intact function of the eye lids.
... accordingly damage or negative influence on gland function and / or on the eyelid function can lead to a "dry" eye condition, i.e. an irritation with all the downstream consequences. if this condition becomes chronic, it can pass into the disease of the "dry eye".
WHY is the surface of the eye so important?
=> The healthy surface of the eyes is a prerequisite for VISION !
The healthy ocular surface allows a clear window for the eye to see the light from the environment.
Without a healthy eye surface, all later steps in the visual process become meaningless.
Deeper INSIGHT into ...The DRY EYE
The DRY EYE is a disorder of the permanent moistening of the surface of the eye with a disorder of visual acuity and subsequent damage to the tissue. This then leads to the patient's complaints and to the clinical findings of the surface damage
What is the DRY EYE?
=> The dry eye is a DEFICIENCY of the constant moistening by the tear film - mostly with subsequent tissue damage
The 'DRY EYE' disease is also medically referred to as " keratoconjunctivitis sicca " (KCS), ie " dryness inflammation of the cornea and conjunctiva " or, shorter, as sicca syndrome (dryness syndrome).
Interestingly, the formation of the oil layer in the tear film is of greater importance than the formation of tear water, because if there is a lack of oil, even abundant tear water evaporates quickly. Gaps are then created in the tear film and the sensitive cells on the surface of the eye are damaged.
Colloquially, the terms 'dry eye' , ' burning eyes ', ' heavy eyelids' or 'tired eyes ' ... as well as many other terms are common, which in one way or another suggest that the surface of the eye is irritated.
The DRY EYE is a complex regulatory disorder of the functional anatomy of the surface of the eye, which reduces the permanent moisture of the tissue and thus its health and perfect visual acuity .
This is typically accompanied by subjective symptoms of various degrees of irritation and pain on the surface of the eye as well as clinical findings of tears and corresponding tissue destruction as well as disorders of visual acuity , mostly in the sense of fluctuating visual acuity or blurred vision.
Rarely, tissue damage can also occur first in a sicca
This happens when the disorder of the tissue surface is caused by another underlying disease. Then a dry eye can appear due to primary tissue damage, which only leads to tear film disorders afterwards. Examples are:
a nutritionally strong vitamin A deficiency or
a local or systemic inflammatory disease
the chronic effect of cell-damaging preservatives in eye drops, especially if they are dripped over a long period of time and several times a day
In more developed countries, systemic inflammatory diseases are more common than primary tissue damage in a sicca. With the increase in bone marrow transplants, the number of rejection reactions in the sense of a ‘ graft-versus-host disease’ (GvdH) , which can also affect the eye and then often trigger a sicca.
In less developed regions of the world, on the other hand, primary tissue damage due to a nutritionally strong vitamin A deficiency is unfortunately still common. The squamous metaplasia of the conjunctiva (see figure) in the emerging sicca is then even used as a diagnostic marker for the vitamin A deficiency.
Symptoms of Dry Eye Disease
What are the typical symptoms of a DRY EYE?
Typical subjective SYMPTOMS are different degrees of eye dryness, blurred vision, eye irritation and pain!
The basic causal factors of insufficient tear production and / or insufficient spread of a (sufficiently stable) tear film ...
... lead to the basic pathologies of the dry eye, namely the instability of the tear film and the subsequent drying and damage to the tissue.
These two pathologies explain the typical symptoms of the dry eye:
feeling of dryness
the feeling of dryness is perhaps the most common and therefore eponymous complaint - although many other symptoms are possible
wet eye
initially there may occasionally be an increased flow of tears and ´ watery eyes´ alternating with dry eyes
... this is triggered by a reflex activation of the tear production - a protective reflex of the surface of the eye
irritation and pain - to varying degrees
sandy gritty feeling, foreign body sensation , burning and stinging
dull feeling of pressure around the eye and even behind the eye is possible
this also explains the common description of the dry eye as:
'heavy' eyelids or ' tired' eyes
' Heavy eyelids' and 'tired eyes ' describe the subjective perception of constant increased friction between the eyelids and eyeball during chronic dryness and tissue irritation
fluctuating visual acuity / blurred vision
Visual disturbances are common and usually consist of occasional blurred vision or fluctuating visual acuity - they result from an uneven thickness of the tear film and are typically improved by blinking several times.
increasing problems with contact lens wear
Since contact lenses place increased demands on the tear film and also the evaporation of the aqueous tears increases, there is an increasing incompatibility of contact lenses , especially soft hydrogel contact lenses
redness
an eye redness is typical in chronic irritation - but usually not very pronounced in mild to moderate dry eye
It is typical of the dry eye that the subjective symptoms do not always exactly match the clinical findings .
Clinical findings
What are the typical clinical findings of dry eye disease ?
Typical dry eye clinical findings are
decreased tears ,
low stability of the tear film , and thus insufficient wetting of the tissue
Damage to the tissue surface leads!
The animated schematic drawing shows a very unstable tear film. Here, after a blink of an eye, it only remains stable for about a second before it opens. This indicates a strong disruption to the system and suggests subsequent tissue damage .
the stability of the tear film is determined by the Tear Film Break-Up Time (BUT)
is typically examined by staining the otherwise largely invisible tear film with a blue-green vital dye (fluorescein)
the normal value should be at least 10 seconds are to the tear film break up and thereby initiating a new blink , which then propagates a new intact tear film.
At the onset of dry eye disease, there may also be occasional episodes of increased lacrimation with watery eyes , which alternate with dry eyes
=> Further information can be found HERE
Defects in the cell surface / vital staining (normal: no staining)
A moderate dry eye typically shows only a slight reddening of the conjunctiva and possibly the edges of the eyelids. The openings of the Meibomian sebaceous glands are often blocked by visible or invisible thickened secretion - this is the most common main cause of the dry eye. Surface defects appear in vital staining with fluorescein as superficial punctate keratitis (KSP).
An unstable tear film triggers dry spots in the epithelium of the surface of the eye due to the frequent, early opening.
There, the surface epithelium is disturbed by two major damage mechanisms ( secondary pathogenetic factors ): increased mechanical friction and increased osmolarity.
The injured, dried cells can be stained on the cornea with the vital dye fluorescein . On the conjunctiva, lissamin green usually stains better. The defects appear as small spots of staining (as keratitis superficialis punctata , KSP) in biomicroscopy with a slit lamp. You can find more detailed information on vital staining => HERE .
=> This vital staining is another important test for the dry eye, since it shows the severity of the dryness of the tissue damage and thus the dry eye.
Aqueous Tear Production Disorder ( Normal:> 10mm )
With moderate to advanced dry eye, the aqueous tear production is often disturbed - either in the sense of a reduced aqueous production or, occasionally, as excessive secretion.
Mostly (in 4 out of 5 cases) in dry eye oil deficiency in meibomian gland dysfunction with subsequent hyperevaporation is the primary cause of dry eye. But damage to the tissue, including the nerve fibers, can lead to disturbances in neural autoregulation of tear secretion.
It is therefore useful to have an orientation impression of the production performance of the lacrimal gland for the watery tears.
The appropriate test for the maximum production capacity of the lacrimal gland is the Schirmer 1 test (without prior local anesthesia). It is therefore advisable to carry out a preliminary determination of the tear film stability and a subsequent vital staining with fluorescein without the addition of a local anesthetic.
REDUCED TEAR VOLUME
on the surface of the eye
(mostly) by increased evaporation of the tear water - as ' evaporative dry eye' called ... or
(much less often) due to a reduced amount of (aqueous) tear secretion from the tear gland
referred to as ´ primary watery tears ´
diagnostic
wird ein effektiver Tränenmangel an der Augenoberfläche am einfachsten festgestellt durch eine Beobachtung oder Vermessung des Tränenmeniskus.
weiterführend sind: Tränenfilm-Tests und Drüsen Tests
ÖL MANGEL
(nach Menge oder Qualität oder beidem) mit Störung der Lipidschicht auf dem Tränenfilm und nachfolgender verstärkter Verdunstung
dies ist eine typische Folge der Meibomdrüsen- Dysfunktion´, (MDD) - sieist der Hauptgrund für ein Trockenes Auge.
Diagnostisch:
lässt sich die Funktion der Meibomdrüsen am einfachsten prüfen durch eine ´Diagnostische Expression´
Genauere Diagnosen und Quantifizierungen werden möglich durch Interferometrie und Meibographie.
Verschwinden von Meibomdrüsen Gewebe
(im Engl. bezeichnet als ´Gland Drop-Out´) bei der optischen Betrachtung (Meibographie) der sonst nicht sichtbaren Meibomdrüsen, die versteckt im Augenlid liegen.
Veränderungen am Lidrand wie:
Schaum und Ablagerungen auf dem Lidrand durch veränderte Fette der Meibomdrüsen
verstärkte Rötung und verstärkte Füllung der Blutgefässe
Demodex Milben an den Wimpern
blocked meibomian gland openings with protrusion or leaked hardened fats of the meibomian glands
Rounding and irregularities of the back edge of the eyelid
Epithelial damage => KSP
Increased friction and increased tear film osmolarity in tear film disorders lead to damage with defects in the surface of the eye. You can find more detailed information on vital staining => HERE .
This affects the surface epithelium first and can be demonstrated by staining with vital dyes . Defects occur:
on the cornea / cornea and conjunctiva / conjunctiva as superficial punctate keratitis (KSP)
but also on the back edge of the lid edge - as a lid wiper epitheliopathy (LWE)
Increased amounts of inflammatory mediators
Inflammation mediators are typically formed by dry eye tissue destruction and occur in tears and tissues. These are various factors, e.g.
inflammatory cytokine and chemokine signaling substances
subsequent activation of tissue-degrading enzymes (matrix metalloproteinases, MMP ).
The most common protease (MMP9) on the surface of the eye can be diagnosed with a rapid test .
Damage to the connective tissue => LIPCOF
If the surface damage progresses and inflammatory reactions occur, the connective tissue underneath the epithelium is also damaged. Here typically occur Li dkanten- P arallele Co njunctivale F old ( LIPCOF on).
LIPCOF are the sign of advanced tissue destruction through the activation of tissue-destroying enzymes , mostly matrix metalloproteinase (especially MMP9).
Due to the tissue destruction, the conjunctiva becomes increasingly looser and ´folds wrinkles´. They already occur due to the low forces of the normal blinking of the eye over the surface of the eyeball. The rear edge of the eyelid then pushes the loosened conjunctiva in front of you like a snow plow when gliding over the globe.
Diagnostically are LIPCOF wrinkles in the slit lamp easily evaluated - better after staining of the tear film with fluorescein.
Nervous system regulation
The surface of the eye is regulated by the nervous system from the peripheral nerves and the central nervous system.
Important functions such as tear secretion and sufficient blinking are automatically regulated by reflex. At least when blinking, there is an arbitrary influence. For example, arbitrarily performed blinking and particularly powerful blinking are possible, which can help to improve the moisturization of the eye.
Stimulus and neural regulation of lacrimation and blinking
The sensory irritation of the surface of the eye in the dry eye, for example through drying, rubbing, hyperosmolarity or injury, reaches the central nervous system (CNS) via the eye nerves (cranial nerve V, trigeminal nerve).
The signals are processed there and the function of the eye is automatically regulated in the brain stem as required.
For example, the flow of tears and blinking are regulated via nerves that run back from the brain stem and brain to the eye (cranial nerve VII, facial nerve).
This also explains why chronic irritation in dry eye occasionally on overshooting irritant secretion and 'Wet eye' can lead
Excessive tear formation is a protective reflex of the eye , in which, in itself, a useful experiment simply ´wash away´ a ´excitement´, like a foreign body on the surface. With chronic irritation in the tissue itself, however, this cannot work.
At the same time, signals also reach the cerebral cortex, so that this can be perceived consciously and can also be reacted to when necessary.
Eyelid regulation - normal, rare or incomplete blinks
The processing of the signals from the surface of the eye is complex and is influenced by various centers in the CNS.
In principle, the blinking is controlled by the blinking reflex. When the tear film on the surface of the eye breaks open, the tissue begins to dry out, irritating the nerve endings there.
This triggers a blink of an eye, which spreads a new, even tear film and thus makes the nerve stimulus disappear again.
The reflex blink of the eye happens largely unconsciously, although a blink of the eye can of course be perceived consciously and also controlled consciously.
Rare eyelid blinks
With increased attention due to strenuous visual tasks, eyelid blinks can be deliberately delayed or suppressed
This affects many everyday activities, e.g. reading , especially on computer screens , watching TV or driving a car , especially at night, etc.
Then the eye is kept open longer so as not to interrupt the 'important' visual impression, even if a dryness stimulus comes from the surface of the eye.
In the illustration, the eye turns red due to the irritation before the blink of an eye finally occurs.
The eyelid blinks can then occur significantly less than the normal value of approx. 5-10 times per minute. Since the tear film is only stable for about 10-20 seconds , the surface of the eye can dry out easily.
So rare blinking can create or worsen dry eyes.
On the other hand, not only the frequency but also the complete sequence of blinking can be influenced.
With ´nervous blinking´ due to lack of concentration, nervousness, or habitually, eyelid blinks can be done more often than necessary and are often incomplete without being consciously noticed.
Incomplete blinking means that the upper eyelid does not close completely when the eyelid is closed (please see animated image). Therefore, the tear film cannot be completely renewed. The lower part of the tear film then always remains relatively dry and there is increased damage to the cell surface .
Incomplete blinking is quite common and is therefore a common co-factor in dry eyes. However, they are not noticed by the patient and are sometimes difficult for the doctor to diagnose without special equipment .
Irritation and processing to feel pain
The neuronal regulation of the surface of the eye, via the cranial nerves V ( trigeminal nerve ) and VII ( facial nerve ) in the brain stem, and also their emotional perception in the brain is complex. It is susceptible to interference, but it can also show certain individual differences between different people. Experiences, evaluations and different types of treatment and processing of events on the surface of the eye are also included here. It is also an experience of everyday life that the ' nerve costume ' can be a little different for every person.
In principle there is a certain difference between the pure ´perception´ of a stimulus from the surface of the eye that occurs in the cortex and the evaluation of these stimuli in the ´subordinate´ Limbic system.
´Pain´ is not a perception in the actual sense, but a construction of the brain .
This construction results from the emotional evaluation of a perception. The evaluation takes place above all in the so-called limbic system and through other emotional instances. Numerous other things, such as experiences and expectations, etc., flow into the subjective evaluation.
However, for the individual person the two instances of ´perception´ and what appears as ´pain´ are not always to be clearly separated. So in the end it is not always clear which of the various instances in the brain is ' cook or waiter ' .
On the surface of the eye, this means that the strength of a stimulus on the surface of the eye and the feelings of pain that the patient perceives subjectively are not always closely related.
Difference between clinical findings and patient perception
Why do the SYMPTOMS of the dry eye often not match the clinical FINDINGS?
=> ... this has not yet been fully clarified and is the subject of current research!
It is typical of the dry eye that the severity of the patient's subjective symptoms in terms of pain does not always match the clinically detectable findings .
Subjective evaluation
Therefore, the subjective evaluation of a stimulus from the surface of the eye can dominate over the objective perception. This can depend on the ´day form´ of the individual person, but it can also be very different for different people.
This can be expressed in such a way that the subjective symptoms cause the patient to suffer a great deal of suffering while little or sometimes no objective findings are clinically detectable - this may be a pain syndrome .
On the other hand, however, a patient with significantly pronounced clinical findings, for example a surface damage that can be stained, may have little or no subjective symptoms in the sense of irritation or pain. Such a patient will then probably have little inclination to medically indicated therapy.
Pain syndrome
Disorder of pain processing can lead to pain syndrome.
Pain has the biological meaning to indicate damage to the body and thus give a signal for danger. With chronic chronic pain stimuli , disorders in the area of the pain system can occur. Routes of transmission of the nerves in the pain system can then be cleared and increasingly solidified. Then pain may persist, even if the pain stimuli on the body decrease or the tissue damage has already healed.
It has lost its actual meaning as a warning signal and becomes part of the disease. These pains are described as “neuropathic” pains
This means that a subjective impression of pain can continue to exist for the patient, even though successful treatment of the dry eye has already improved the condition of the surface of the eye.
Psychosomatic influences
Psychosomatic influences on a disease process and on the patient's perception have been an established and serious part of medicine for many years. In addition to, for example, non-specific back pain, functional cardiovascular problems or indigestion, this can also play a role in the dry eye , according to many studies .
If dealing with the disease becomes the most important part of life, this could be an occasion to seek psychosomatic help .
HOW does a dry eye develop?
... and how does it become CHRONIC? ? ?
Dry eye is strongly influenced by regulatory systems and risk factors
Various factors influence the function of the surface of the eye
A disruption of positive factors and the appearance of negative factors (risk factors) worsen the normal functioning of the tissue and therefore increase the risk of the appearance of a dry eye and the severity of the disease.
The complex disturbance of the function and structure of the surface of the eye in the dry eye leads to a lack of the basic functional complexes for the constant moisturization of the tissue.
The development of a dry eye is favored by several factors:
REGULATORY SYSTEMS
Disruption of regulation
Disorders of the nervous system, the endocrine hormone system and the immune system impairment the function of the surface of the eye.
Age and female gender (in connection with a relative lack of 'male' androgen hormone and an excess of 'female' estrogen) have a significant influence on the surface of the eye.
EXTERNAL RISK FACTORS
mostly have a drying effect
Negative external influencing factors are RISK FACTORS for the disease. They affect the TEAR FLUID on the eye and over claim the normal function capacity - but are often easily influenced. It is mostly drying environmental influences such as heat, drought, wind - even concentrated visual tasks with rare blinking of the eye. In climatic-ized office environments with VDU these risk factors are often combined and may be so for dry " office eye " (Engl. " Office Eye cause").
INTERNAL RISK FACTORS
Disorder of the organs
Negative internal influencing factors are also RISK FACTORS for the disease.
They affect the TISSUE that produces the tears and can worsen the normal function of the surface of the eye.
These are, for example, age and gender, as well as chronic illnesses or chronic medication, nutrition and drinking volume etc.. Many of these internal risk factors are difficult to influence.
Why does the dry eye tend to get worse?
... without adequate therapy
=> Tear deficiency with reduced moistening of the eye surface and subsequent tissue damage have a negative impact and reinforce each other!
Self-reinforcing inflammatory mechanisms
The complex pathological changes in the dry eye influence each other and form self-reinforcing control loops, which are often referred to as vicious circles.
This often leads to exacerbation of the disease if insufficient therapy is given.
Inflammation is an important enhancement mechanism
Inflammation is a powerful mechanism for the exacerbation of dry eye disease.
Inflammation is a basic mechanism for cells to defend themselves. against wounding and damage. This also typically occurs in dry eyes due to the instability of the tear film and the subsequent increased mechanical friction and increased osmolarity of the tear film.
Inflammation mechanisms cause tissue destruction to overcome the supposed pest and should then lead to tissue repair.
In diseases like the dry eye, ongoing tissue damage can lead to chronic inflammation.
If the inflammation becomes chronic, then it turns into a negative and destructive process because the initial tissue destruction cannot be replaced by an adequate repair and thus becomes increasingly severe. This creates self-reinforcing control loops (' vicious loops ') of worsening of the disease.
This powerful mechanism can significantly worsen the disease process.
In such cases of moderate to severe dry eye, it often makes sense if the treatment contains temporarily anti-inflammatory therapy approaches in addition to tear substitutes and physical lid margin therapy with lid margin hygiene .
For detailed information about dry eye therapy, we refer to the longer English language version of the OSCB information portal.
When does a "dry" eye become dry eye disease?
If a ´dry´ eye becomes chronic - then an occasional, temporary disorder can develop into a chronic DISEASE!
An occasional “dry” eye is not a disease
Most of us have probably already had a temporary feeling of 'dry' eyes, for example when we were exposed to unusually strong drying environmental influences. These are, for example, low air humidity, high temperature, wind, or rare blinking when working concentrated in air-conditioned room air.
Such a ´dry´ eye is typically a short-lived condition, which quickly improves and disappears when we become aware of it and increasingly blink or leave the drying environment.
When “dryness” becomes chronic ... this condition can turn into a disease
Only if the feeling of 'dryness' persists and cannot be improved by avoiding drying out environmental factors and by increasing, consciously and intensely blinking ...
… Then the temporary condition becomes chronic and an occasional “dry” eye can progress to the disease of the dry eye.
This is typically associated with an increase in the DURATION and SERIOUSity of symptoms and clinical findings due to increasing disruption and damage to the surface of the eye. Some important risk factors favor the appearance and severity of the dry eye.
Many different and mutually influencing self-reinforcing control loops of the exacerbation of the disease (often referred to as ´Develskreise´, English ´VICIOUS CIRCLES´) occur in the chronic dry eye and can lead to the clinical full picture of a chronically progressive tissue destruction with a loss of function of the eye surface to lead