Diagnosis 4
Tissue Damage at the Ocular Surface
Main causes of epithelial disorders and surface damage
Epithelial damage typically occur when the normal health of the ocular surface is compromised to an extent that it leads to symptoms. Epithelial damage is caused by two main factors, namely by increased mechanical friction due to dryness, i.e. the lack of 'lubricant' between the eyeball and eyelids, and by increased osmolarity, i.e. an increased concentration of salts and proteins in the remaining tears when the tear water evaporates due to oil deficiency.
Chronic Mechanical Friction and Hyperosmolarity presently appear as the main Secondary Pathogenetic Factors due to and downstream of Tear Film Deficiency. Surface Damage, starting with the Epithelium, induces another sequence of downstream secondary pathogenetic factors, that lead to inflammatory reactions. In chronic stages this can lead to chronic destruction of the Ocular Surface Tissue in severe Dry Eye Disease. This Pathophysiology of Dry Eye Disease is explained in more detail in the Animation on the HOLISTIC DYNAMIC CONCEPT on the PATHOPHYSIOLOGY in Dry Eye Disease.
Going along the Pathophysiology of Disease ... makes the understanding of pathology and of therapy much easier
Even though chronic mechanical friction and hyper-osmolarity are certainly important factors in Dry Eye Disease, in a pathophysiological view on this disease condition, they are no primary events but they arise due to other prior events such as tear film deficiency ... and that in turn is again based on other basic causative factors such as gland dysregulation etc.
A pathophysiological view in medicine is however not an academic fooling around ... but instead is the approach that leads to understanding of the causative relations of the condition and thus of likely successful therapy approaches.
This is the reason, why the new HOLISTIC DYNAMIC CONCEPT on the PATHOPHYSIOLOGY of DRY EYE DISEASE is strictly based on the pathophysiological course... and, also, what is thought to be ´important´ today may very well change already by tomorrow.
Increased Mechanical FRICTION is a main pathogenetic factor for Ocular Surface Disease. Friction occurs during all movements of the eye ball relative to bony orbita and the lids, particularly during blinking. Pathologically increased friction occurs when the normal lubrication by the tear film is reduced due to the pathology in e.g. Dry Eye Disease or due to external factors such as a contact lens.
increased FRICTION
an unusually strong mechanical friction
typically between the bulbar mucosa (cornea and bulbar conjunctiva) and the palpebral conjunctiva of the eye lids
that exceeds the normal level of friction
which necessarily occurs by eye movements and blinking
but is limited to a tolerable degree by several lubrication systems
due to additional influence factors such as e.g.
a lack of tear water (aqueous tears) as e.g. in Dry Eye Disease, desiccating environments etc.
a lack of mucins due to squamous metaplasia as e.g. in Dry Eye Disease
additional external factors such as e.g. a contact lensthat can lead e.g. to Dry Eye Disease
The schematic drawing illustrates the impact of a local spot of hyper-osmolarity that may occur e.g. due to a local break-up of the tear film with local evaporation of water and accumulation of the remaining tear salts and proteins (gray spots). The hyper-osmolarity drags water from the epithelial cells with potential shrinkage and cell disruption. This represents a danger signal and activates an inflammatory response with production of inflammatory mediators. In chronic conditions and with wide-spread hyper-osmolarity a pro-inflammatory milieu may build up that can lead to the onset or promotion of Dry Eye Disease. (for schematic reasons the local hyper-osmolarity zone here is much too small because it may be assumed that even a small local hyper-osmolarity will affect several or many cells at a time).
CHANGES in OSMOLARITY - typically Hyper-Osmolarity
an unusually strong deviation of the osmolarity of the luminal tear fluid from the normal value of just under 300mosm/l (MilliOsmol per liter) - => as explained there
typically by increased evaporation of aqueous tears
due to a lack of tear film lipids
in obstructive Meibomian gland dysfunction (MGD)
in low blinking frequency with low delivery of lipids from the glands
in desiccating environments
with subsequent concentration of salts and osmotically active functional proteins
that may occurs at least in local spots of hyper-osmolarity
this exerts a hyper-osmolar stress on the epithelium
that drags out the water of the epithelial cells and can lead to surface damage and activation with onset of an inflammatory reaction.
Increased FRICTION and Increased OSMOLARITY are the two main secondary pathogenetic impact factors for the occurrence of EPITHELIAL DEFECTS.
Friction occurs mainly at the bulbar surface inside the palpebral fissure and at the palpebral posterior lid border, mainly in the upper eye lid but also to a certain extent in the lower lid. Under normal conditions there is enough lubrication available by a sufficient amount of tear fluid and additional lubricative proteins such as lubricin. In conditions of increased friction, such as in Dry Eye Disease and Contact lens wear the normal movements of eye ball and lids against each other already cause epithelial damage. This can be made visible by ´Vital Staining´using different stains because the wounded cells pick up the stain and the normal ones don´t. The staining at the eye ball is termed as corneal or conjunctival staining or superficial punctate keratitis or just as ´Vital staining´. The vital staining of the elevated epithelial lip of the lid wiper zone at the posterior lid border is termed Lid Wiper Epitheliopathy (LWE) by KORB and colleagues.
Epithelial defects in Dry Eye Disease typically occur
at the BULBAR surface, as explained, but also occur
in the PALPEBRAL region of the Lid Wiper
at the posterior lid margin where the frictional forces of the upper lid appear to be concentrated. Lid Wiper Epitheliopathy (LWE) with pathological vital staining was observed to be the most sensitive indicator for increased friction at the ocular surface.
This little collection of the main pathogenetic factors does not include more severe impacts such as dramatic changes of the external milieu e.g. in ocular burns due to aggressive chemicals or all sorts of accidents or serious infections that can all happen but are less frequent than chronic mechanical friction and local hyper-osmolarity.
A schematic drawing indicates the image of fluorescein stained epithelial alterations that occur as small dots. The size of the stained dots, that originate from single stained cells in principle, is somewhat too large here in the drawing in order to make them better visible. Specific patterns of staining can occur such as here band-like within the palpebral fissure. Staining patterns may each allow proposals on the mechanism of pathogenetic alteration.
The visualization of staining of epithelial defects is an established cornerstone of Ocular Surface Diagnosis in general and particularly of Dry Eye Disease. Different stains are used and applied in the clinic directly onto the living, vital Ocular Surface Tissues without doing any harm them them - except for sometimes a mild irritation. Since these vital stains are used topical at the ocular surface, they are sometimes also termed ´topical´ stains.
Such stains that are clinically applied to living tissues are termed ´vital´stains which is probably best understood as opposed to histological stains that are typically applied to avital, fixed and thus dead cells and tissues in cytology and histology. The term ´vital´ therefore applies to the stained tissue but not to the stain itself, because some staining chromophores can be used in vital staining as well as in histology - this applies for example to lissamine green.
A schematic drawing at the cellular level indicates the image of fluorescein stained epithelial alterations that occur as small dots. The stained dots that originate from single stained cells in principle, are shown here a polyhedral objects. Often pathogenetic impacts on the epithelium, due to e.g. friction or hyper-osmolarity. will affect more than one individual cell in a place, so that the stained spots may become larger than one cell diameter.
Staining Principle
The staining principle is, that the binding of substances by living ocular surface tissue is typically inhibited or limited or only short term due to e,g, the washing effect of the tears or due to the mucin layer.
Therefore only areas of the ocular surface where the normal integrity is altered in any way will bind stains and such alterations are thereby made visible.
The surface alteration can be either on the cellular level by wounding and disruption of cell membrane integrity or (only) on the extra-cellular mucin level by alteration or disruption of the mucins.
Vital staining typically occurs in the form of small dots that are only detectable by magnification in a slit lamp.
The severity of ocular surface staining that occurs due to pathological epithelial alterations is typically determined according to the amount of stained cells. The location also appears to have some significance because nasal staining (top image) is typically mild and unspecific, whereas temporal staining (bottom image), i.e. in a location where the fresh tears pour out of the excretory lacrimal ducts into the conjunctival sac, typically indicates a more severe condition and is somewhat specific for Dry Eye Disease (Schematic drawings according to observations of UCHIYAMA and colleagues 2009).
Staining CONCEPT
The general concept is that increased staining corresponds to increased alteration of the surface integrity and thus corresponds to and indicates an increased pathological impact and increased disease severity. The more stained dots occur after vital staining the more the ocular surface damage and thus the disease severity is.
As explained in the chapters on the ´Basics of Function and Disease´ and on ´How Dry Eye Disease gets Worse´ the pathological alterations of the epithelium are basically negative effects of desiccation and they occur mainly by the Secondary Pathogenetic Events of:
to chronic mechanical friction due to decreased lubricative activity of the reduces tear film
chemical irritation of a hyper-osmolar type due to increased evaporation of aqueous tears
Staining LOCATION
It can be assumed that most of the surface cell destruction will occur in the region that is exposed to the ´dry´ ambient air in the bulbar area of the inter-palpebral fissure, where we have to open our eye lids in order to let the light in, that we need for the primary function of the eye ... which is of course vision.
Indeed most staining occurs in the inter-palpebral fissure area of the eye ball and therefore affects mainly the cornea and a part of the bulbar conjunctiva.
It may further be assumed that the tissue destruction, that is based on desiccation, occurs preferably where least tears occur on the ocular surface.
This would be away from that side where the excretory ducts of the lacrimal gland enter the conjunctival sac (temporal side) and thus more surface damage may be assumed on the nasal side.
Indeed experienced ophthalmologists seem to verify this assumption, because, e.g the group of James McCULLEY from Dallas reported in the Ophthalmology Newsmagazine 2008, that vital staining in the nasal area occurs more frequently and is not necessarily specific for Dry Eye Disease but the occurrence of a temporal vital staining indicates a more severe dry condition and is relatively specific for Dry Eye Disease.
BULBAR Epithelial Defects - Vital STAINING
Staining Scores - Oxford ScORE
VITAL STAINING of Epithelial Alterations of the Ocular Surface is typically evaluated in a semi-quantitative fashion by estimating the amount of staining, which is basically equivalent to single stained cells, by comparison with a chart that shown certain model grades. A popular Grading System is the OXFORD SCORE because this is easy to use and produces relatively reliable results. The staining intensity shown here schematically represents a medium (grade 2) staining on the Oxford Scale.
The amount and often distribution of staining is estimated according to different scoring systems, of which the OXFORD Score is probably most frequently used.
The Oxford Score records the intensity of staining, i.e. the amount of stained dots, separately for the nasal and temporal conjunctiva and for the cornea.
The severity of staining is then scored in six grades of increasing severity from 0 to 5 with the assumption that the staining is expressed more or less uniformly over the three mentioned areas.
The evaluation is done in a semi-quantitative fashion by comparing the staining in a individual patient with the six grades of the scoring chart that shows a schematic representation of each of the different staining images - the closest match between the patient´s result and the chart does then determine the classification. This system is relatively reliable and easy to perform and is often used for studies.
Disparity of Signs and Symptoms in Dry Eye Disease
... sooo easy could be the life of a clinician and of a patient IF this was already the full picture. In Dry Eye Disease, however, it often occurs that there is a certain disparity between such objective clinical signs as vital surface staining and the subjective symptoms of an individual patient. This may be based on aspects of neurobiology on any level that may influence the uptake, transmission, or central computation and reception of neural signals ... as discussed elsewhere.
PALPEBRAL Epithelial Defects - Vital STAINING - Lid Wiper Epitheliopathy (LWE)
Friction occurs mainly at the bulbar surface inside the palpebral fissure and at the palpebral posterior lid border, mainly in the upper eye lid but also to a certain extent in the lower lid. The elevated epithelial lip of the lit wiper at the posterior border wipes for a distance of about 10mm back and force over the bulbar surface during each of the frequent blinks. The frictional force that occurs is here concentrated on a relatively small surface whereas the same friction on the other (bulbar) side is distributed over a much larger are. Normally the friction is sufficiently limited by a sufficient tear volume and by a rich mucin-water gel that is enriched on the Lid Wiper Surface by many goblet cells and goblet cell crypts (indicated in the 2 images on the right side). In conditions of increased friction, such as in Dry Rye Disease and in Contact lens wear a pathologically too high mechanical friction and thus alteration and wounding of the epithelium will first occur at the lid wiper. This is indeed true because it was observed by KORB and colleagues that Lid Wiper Epitheliopathy (LWE) is the first area if vital staining in elevated friction conditions.
Friction also occurs at the palpebral posterior lid border
Vital staining of epithelial alterations does not only occur at the bulbar surface which is the typical region for evaluation of ´ocular surface´ vital staining, e.g. according to the Oxford Score.
In conditions with increased friction at the ocular surface, such as e.g. in Dry Eye Disease and in Contact Lens Wear, also the palpebral conjunctiva suffers epithelial defects that can be visualized by vital staining.
This concerns specifically the marginal conjunctiva at the palpebral aspect of the posterior lid border - termed the LID WIPER. This zone is apposed and directly in contact to the globe whereas the rest of the tarsal conjunctiva is separated from the eye ball by the narrow tear lake of "Kessing´s space".
The elevated epithelial lip of the Lid Wiper is that part of the eye lid, that wipes over the bulbar bulbar surface during a blink. Thereby the Lid Wiper compresses the ´old´tear film, that frequently already has thin areas or even disruptions, during the down-stroke of the upper eye lid. During the up-stroke of the lid the lid wiper spreads out a new tear film (please see the animation below).
The frictional forces during the blink concentrate on the Lid Wiper
Therefore most or almost all of the frictional forces of the eye lid rest on the lid wiper zone whereas the friction of the bulbar conjunctiva is distributed over a wide area. In conditions with increased friction at the Ocular Surface the Lid Wiper is consequently the zone where most alteration and wounding will occur.
In fact vital epithelial staining of the lid wiper zone - termed as LID WIPER EPITHELIOPATHY and abbreviated as LWE - was reported as a very sensitive first indicator of increased friction in patients with Dry Eye Disease and in Contact Lens Wearers by KORB and colleagues in several reports since about the millennium years.
LEW already occurred when conventional markers for Dry Eye Disease, such as short Tear Film Break-Up Time (BUT) or Schirmer´s Test were still normal or borderline normal. Patients with Dry Eye Disease, which includes respective symptoms, overwhelmingly (about four fifth) have LEW whereas patients without respective dry eye symptoms only rarely have LEW of any degree. LEW therefore represents an important and very specific indicator for elevated mechanical friction at the Ocular Surface.
Grading of Lid Wiper Epitheliopathy is made according to the extension of alterations
The severity of LWE is graded according to the extension of the vital staining in two dimensions - vertical hight and horizontal width - in 4 Grades from 0 to 3 - as explained by KORB and colleagues 2010 in the Cornea Journal:
the vertical height is graded as:
in parts of the LW height
25% 0 (normal)
25% to 50% 1 (mild)
50% to 75% 2 (moderate)
75% 3 (severe)
the horizontal width is graded as:
< 2 mm 0 (normal)
2–4 mm 1 (mild)
5–9 mm 2 (moderate)
> 10 mm 3 (severe)
The mean value for both dimensions makes up the total grade of LWE.
OPTIMAL VITAL STAINING of LWE
LWE stains with all ordinary chromophores that are discussed here - Fluorescein, Lissamine Green and Rose Bengal.
The intensity of vital staining can be optimized by mixing 2% fluorescein with 1% Lissamine Green and for applying one drop (40µl) for each eye two times with 5 minute interval. The staining can be analyzed one minute after the second drop.
Different Vital STAINS
There are different vital stains that are often used interchangeably even though the have slightly different staining principles.
FLUORESCEIN Vital Staining of the Lid Wiper Epithelium of the marginal Conjunctiva. The staining is intensely bluish-green. Fluorescein stains the pathological Lid Wiper Epitheliopathy (LWE) but it is also lying on the tarsal conjunctiva in the middle of the image and partly demarcates substructures such as crypts and other surface irregularities. This superimposition of fluorescein on the epithelium is not a real staining because, as seen in the next image with Lissamine Green staining, the tarsal conjunctiva in such patients is typically unaltered and healthy.
Fluorescein:
Most often used in ophthalmological practice is probably Fluorescein a fluorescent molecule with blueish-green color in the slit lamp. A major advantage is certainly that Fluorescein is a multi-purpose stain that can be used:
for the observation of ocular surface integrity in terms of epithelial alterations - often simply called ´vital staining´
Fluorescein is better suitable for the study of corneal alterations whereas the bulbar conjunctiva, that equally suffers from the pathology e.g. in Dry Eye Disease, stains more weakly
the visibility of Fluorescein can however be improved by using specific filters for excitation (blue) and for observation (orange)
for observation of the tear film integrity in the Fluorescent Break-Up Time Test (F-BUT)
for assistance in contact lens fitting ... which is however safest for RGP since soft hydrogel lenses may pick up the stain
for easier observation of the tear meniscus hight (TMH) ... when it is made sure that the applied volume is minute enough inorder to avoid erroneous reading of a high TMH although this is in fact low
A triple approach is possible with fluorescein:
Since fluorescein stains EPITHELIAL ALTERATIONS and also the TEAR FILM it can be used for several investigations:
first for evaluation of the tear film with respect of BREAK-UP TIME (BUT) and
Tear MENISCUS Height (TMH) and afterwards, when fluorescein is immersed for some minutes, typically 5min, it can be used for
evaluation of EPITHELIAL ALTERATIONS ´vital staining´
... this is a time saving practical approach in ophthalmological clinics.
LISSAMINE GREEN Vital Staining of the Lid Wiper Epithelium of the marginal Conjunctiva. The staining is intensely dark-green and stains the conjunctiva very well and intense. Here it makes the pathological Lid Wiper Epitheliopathy (LWE) visible since the conjunctival cells, that are altered in conditions of increased friction such as Dry Eye Disease and Contact Lens Wear, pick up the stain whereas the other normal conjunctival cells on the tarsal conjunctiva in the middle of the image do not stain.
Lissamine green
Lissamine stains, as its name says, in green color and binds to altered and dead cells e.g. in Dry Eye Disease
it stains the bulbar conjunctiva better than fluorescein
for tear film analysis Lissamine green is not of much use and therefore basically restricted for cellular alterations
ROSE BENGAL Vital Staining of the Lid Wiper Epithelium of the marginal Conjunctiva. The staining is intensely reddish-pink. Vital staining of the Lid Wiper is pathological and termed Lid Wiper Epitheliopathy (LWE), whereas the staining for the thin line (arrows) at the outer aspect is normal and indicates the physiologically stainable Line of MARX.
Rose bengal
Rose Bengal has a reddish to pink color and it is probably best known by the patients because its topical application leads to a distinct stinging sensation
it has a similar staining spectrum as Lissamine green, i.e. it is more suitable for conjunctival alterations
in contrast to Lissamine, Rose Bengal also stains mucins and healthy cells in addition to altered ones, when it has access to healthy cells due to gaps in the mucin layer. These characteristics can make Rose Bengal staining interpretation somewhat more difficult compared to lissamine green and fluorescein.
Vital Stains - Summary:
Fluorescein is the multi-purpose vital stain for the ocular surface and tear film whereas Lissamine Green is preferable for investigation of the conjunctiva, because it stains conjunctival alterations more intensely. Due to the stinging sensation of Rose Bengal, this may only be necessary for very specific purposes.
The intensity of vital staining can be optimized (e.g. for vital staining of Lid Wiper Epitheliopathy of the marginal conjunctiva) by mixing 2% fluorescein with 1% lissamine green and for applying one drop (40µl) for two times with a 5 minute interval. The staining can then be analyzed one minute after the second drop was given.
Since Fluorescein is described as a more intense stain for Cornea whereas Lissamine Green is preferred for the Conjunctiva the described combination of both stains should reveal optimal vital staining results in both epithelia.
A potential challenge may occur because the illumination may need to be switched because fluorescein is best seen with blue light whereas Lissamine Green is best seen in normal white light.
MUCOSAL Status - Conjunctival Stroma
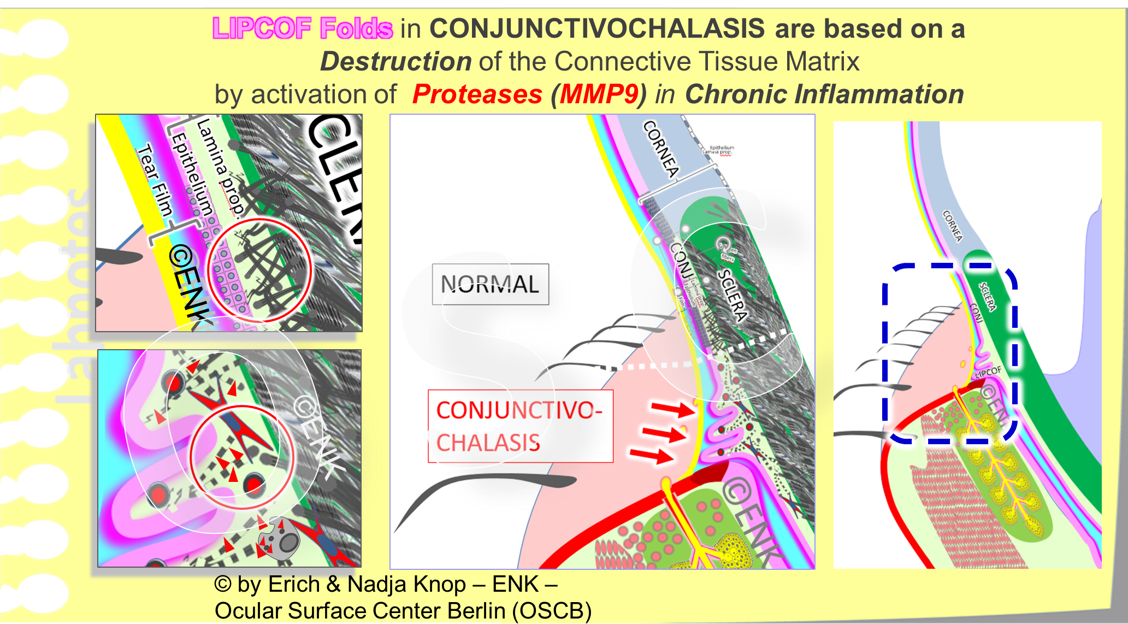
Conjunctival Status - Lid-Parallel Conjunctival Folds (LIPCOF) in chronic Dry Eye
A schematic drawing of an eye with several Lid Parallel Folds (LIPCOF, indicated by arrows) superimposed over the posterior lid border inside the tear meniscus (blue arrows). (The lid margins are slightly everted to show the free lid margin with the tear meniscus)
Lid-Parallel Conjunctival Folds, mostly abbreviated as LIPCOF, are an important pathological clinical sign in chronic Dry Eye Disease.
LIPCOF folds reflect a loosening of the conjunctival tissue (termed conjunctivochalasis). They occur due to increased friction together with high levels of collagen degrading Matrix-Metalloproteinases (MMP), mainly of the type MMP9, in the inflammatory process during chronic Dry Eye Disease.
The loosening is termed conjunctivochalasis from the Greek word χάλασις ("chalasis") for loosening). Conjunctivochalasis describes a general loosening of the conjunctival tissue, whereas LIPCOF folds are the specific phenomenon of the formation of folds chalatic tissue over the posterior eyelid border.
The conjunctival folds were discovered and termed as LIPCOF by Frank SCHIRRA during his PhD study with Prof. Höh in the mid 1990s. LIPCOF form in parallel orientation along the eyelid margin and are most prominent in temporal position (please see figure).
With increased damage of the conjunctival tissue the number and size/ height of the folds increases. The LIPCOF folds typically superimpose and form stacks and can protrude over the surface of the tear meniscus (see figure).
The severity grade of LIPCOF - and thus of dry eye - is classified according to the height of the folds on the temporal lower lid margin.
Frictional forces on the bulbar conjunctiva occur basically during every movement of the eye ball within its nice and cozy mucosal tissue shell behind the eye lids, e.g. during every position of gaze and by fixation of moving objects. Of particular importance is the movement of the eye lids over the eye ball during the blink, because this occurs most frequently, covers a long contact area and also exerts the mechanical force of the lid tension onto the eye ball (please see the animation below). This applies mainly to the upper lid that travels more than one hundred meters a day over the eye ball but also the lower lid exerts some movements along the eye ball.
The formation of LIPCOF conjunctival folds is promoted by increased friction. This is caused by the reduced lubricating effect of the deficient tear film.
Increased friction has an effect on the movements of the eyeball during eye movements and especially during frequent eyelid blinking (see animated figure).
This leads to an inflammatory reaction of the conjunctiva, which is initially subclinical, i.e. invisible. However, inflammatory mediators including tissue-dissolving proteinases are already released, which together with the increased friction lead to LIPCOF folds
In summary, causative ralations can be characterized as follows:
tear film deficiency => reduced lubrication => increased friction => damage and activation of epithelial cells
increased activation of proteases => damage to the conjunctival stroma => conjunctivochalasis
conjunctivochalasis + increased friction = LIPCOF
LIPCOF folds are, as the term behind the abbreviations tells, a very specific form of conjunctival folds - they are ´Lid Parallel Conjunctival Folds´.
The damaged and loosened (´chalatic´) conjunctival tissue tends to be moved back and forth by the posterior eyelid margin during every blink and gradually forms conjunctival folds in front of the advancing lid margin.
The mechanism of LIPCOF formation s similar to a snow plough that pushes loose snow in front of it. This gradually causes conjunctival folds to form on the posterior eyelid margin. They are more visible on the lower lid margin than on the upper lid margin, due to the orientation of the eyelids.
Since conjunctival LIPCOF folds are a typical and obvious consequence of conjunctivochalasis these two terms are occasionally used as synonyms, which may not be quite correct.
Lid-Parallel Conjunctival Folds (LIPCOF) occur when the structural collagen meshwork of the conjunctival connective tissue (Lamina propria) is degraded by proteinases, mainly Matrix-Metalloproteinase 9 (MMP9). The loosening of the conjunctiva is termed ´conjunctivochalasis´. MMP9 is increasingly activated during the chronic inflammatory process in Dry Eye Disease. The loose conjunctiva is then ´shoveled up´ by the relatively sharp posterior lid border and folds up onto the posterior lid border. For simplicity, a zone with ´NORMAL´ collagen structure is shown here directly besides the ´CONJUNCTIVOCHALASIS´. It must however be assumed that the whole conjunctiva is relatively homogeneously affected by this destruction in Chronic Dry Eye Disease.
LIPCOF can be applied for the Severity Grading of Dry Eye Disease
Depending on the progression of Dry Eye Disease also the degree of conjunctival destruction increases and the number and size of LIPCOF folds increases. First there is only one small fold that is barely detectable but later the folds increases in size, they protrude onto the mucocutaneous junction of the posterior lid border i.e. on the bottom of the tear meniscus.
In advanced stages several folds are superimposed - one on the other - and can protrude over the tear meniscus into the ambient air. This leads to drying of the exposed tissue surface and thus to irritation and pain.
Since the degree of LIPCOF folds increases with increasing severity of disease, the fold are an important clinical sign and can be applied for the classification of severity of Dry Eye Disease.
LIPCOF - Severity Grading (according to Schirra and Höh)
The grading differentiates 4 steps:
(Step 0: no LIPCOF folds = Normal)
Step 1: small fold within tear meniscus
Step 2: large fold up to the height of the tear meniscus
Step 3: large fold with sub-folds above tear meniscus
Step 4: large fold, that protrudes over the inner lid border
LIPCOF folds are lying on the posterior lid border and in advanced stages they are superimposed on each other. The lowest, i.e. first fold is typically the largest and protrudes widest in anterior direction whereas the following folds tend to decreased in size with each fold.
Thereby LIPCOF are lying within the tear meniscus and fill it increasingly and thus push up the apparent upper end (height) of the meniscus.
The apparent Tear Meniscus Hight (TMH) is measured or just semi-quantitatively evaluated in order to have an impression of the meniscus filling and thus of the tear volume on the ocular surface.
Therefore, the presence of at least extensive LIPCOF can lead to wrong, i.e. erroneously high readings of tear volume. These observations were published by Pult and Pult.
MMP9 (Matrix-Metalloproteinase 9) is a Tissue Protein degrading Enzyme
Inflammation in chronic Dry Eye Disease can typically induce a progressive damage of the tissue.
Figure-Legend: The basic structure of the CONJUNCTIVA is composed of a loose, but still sufficiently solid, meshwork of collagen fibers. In the clefts between the fibers stromal cells and cells of the innate and specific immune system lead their daily life together with bypassing support structures such as blood vessels (left middle), lymph vessels and nerve fibers (faint yellow lines). MMP9 cleaves the long collagen fibers into fragments and thus destroys the structural basis of the tissue in the praiseworthy attempt to provide more space for the protective ´inflammatory cells´. Problems only occur when the inflammation becomes chronic and thus undermines all attempts for a final ordered repair of the tissue ... which results in a constant conjunctival destruction and thus tissue loosening termed conjunctivochalasis
Even if visible damage has not yet occurred, increased amounts of tissue degrading enzymes may already be present and damage the eye surface.
These are typically matrix metalloproteinases (MMP). In dry eye, the subtype matrix metalloproteinase 9 (MMP9) is particularly important.
A clinical test is available for this important disease factor, which breaks down the tissue of the ocular surface.
The damage to the connective tissue structure of the conjunctiva by MMP9 is shown in a schematic figure.
The tissue-dissolving enzyme MMP9 is secreted and activated as part of the actually protective inflammatory response. This is intended to create space for an effective inflammation to switch off an occurring stimulus.
However, the chronic irritation in dry eye causes a continuous and massive activation of MMP-9 and no normal repair or healing can occur, as biologically intended.
Matrix-Metallo-Proteinases (MMP) are important inflammatory mediators
They are produced and activated downstream of the primary inflammatory mediators such as inflammatory lipids, including eicosanoids, histamine, and inflammatory cytokines that are produced due to the influence of a pathogenic insult onto the tissue.
The pathogenic insult, that is regarded as “danger”, comes typically from the outside and causes tissue damage. This applies e.g. to increased mechanical friction, hyper-osmolarity, Infektion or other damage. Increased mechanical friction due to low lubrication and hyper-osmolarity due to increased aqueous evaporation typically occur in Dry Eye Disease and hit the epithelial cells that appear to be the first producers of inflammatory mediators such as cytokines.
Matrix-Metallo Proteinases dissolve the collagen matrix of the tissue
Lid-Parallel Conjunctival Folds (LIPCOF) occur when the structural collagen meshwork of the conjunctival connective tissue (Lamina propria) is degraded by proteinases, mainly Matrix-Metalloproteinase 9 (MMP9). The loosening of the conjunctiva is termed ´conjunctivochalasis´. MMP9 is increasingly activated during the chronic inflammatory process in Dry Eye Disease. The loose conjunctiva is then ´shoveled up´ by the relatively sharp posterior lid border and folds up onto the posterior lid border. For simplicity, a zone with ´NORMAL´ collagen structure is shown here directly besides the ´CONJUNCTIVOCHALASIS´. It must however be assumed that the whole conjunctiva is relatively homogeneously affected by this destruction in Chronic Dry Eye Disease.
Since an inflammatory reaction is a basic protective answer of tissues, it is necessary to mount downstream mechanism in order to promote this answer.
Apart from up-regulation of adhesion molecules e.g. on vascular endothelial cells to get more ´helpful inflammatory cells´ into the tissue
there is also more space needed within the narrow tissue clefts of the collagen fiber matrix to accommodate the large amount of incoming cells in order to do their job as good as they can.
Proteases are thus activated that can degrade the matrix of the stromal connective tissue of the ocular surface which is mainly formed of proteins, overwhelmingly of collagen fibers (as shown in the figure. Collagen fibers form the structural meshwork in which the stromal cells and support structures such as blood and lymph vessels and nerves reside. At the ocular surface in Dry Eye Disease mainly the Matrix-Metalloproteinase MMP9 is of importance and shown e.g. by Steven PFLUGFELDER´s group, by MELLER and TSENG, and by others.
Conjunctival LIPCOF folds are a clinical sign of chronic MMP9 activation and tissue destruction
Chronic activation of proteases such as mainly the subtype termed Matrix-Metalloproteinase MMP9 leads to progressive tissue destruction alternating with frustrate attempts for tissue repair, which is the final step of the physiological inflammatory process.
The repair attempts with reformation of collagen is unluckily frustrate since the tissue destruction by activation of MMP9 is chronically ongoing.
A convenient test for determining the level of the protein-destroying enzyme Matrix-Metalloproteinase 9 (MMP9) became available. It indicates by an immune-assay based color reaction whether the MMP9 level is over the normal range. The MMP9 test can thus indicate the presence of a chronic tissue destroying inflammatory process that would require therapeutic intervention, even when clinical signs of tissue destruction have not yet occurred. The MMP9 test may thus offer a new preventive approach in Dry Eye Disease.
A rapid diagnostic test is available that can detect elevated MMP9 enzyme protein concentrations.
This is a convenient test that can be performed directly on the patient in the practise. It requires only the collection of a few tears and some superficial cell material from the connective tissue in the lower fornix.
The MMP9 enzyme protein test works by producing an immune reaction, which becomes visible by the appearance of a color reaction when the test is positive, similar to a pregnancy test.
This convenient new test allows the detection of elevated MMP9 levels, and thus of inflammation, before harmful clinical symptoms have occurred such as a loosening of connective tissue with LIPCOF folds.
Such a clinical MMP9 test could therefore offer a chance for a preventive aspect in dry eye.
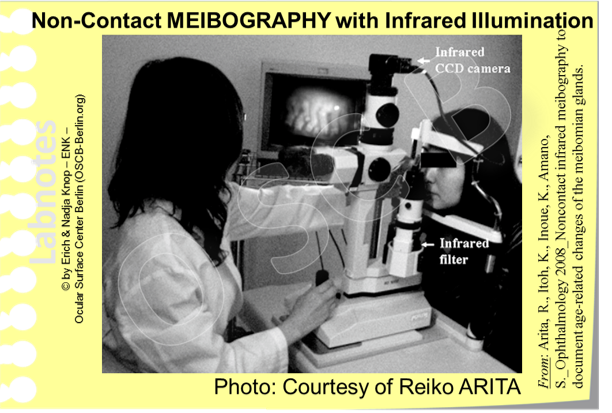
Meibomian Gland Status - Meibography
The interest in the Meibomian Glands has strongly increased after it was publicly realized that a deficiency in Tear Film LIPIDS due to a mainly obstructive Dysfunction of the Meibomian Glands in fact appears presently as the main causative factor for Dry Eye Disease. This may appear a a surprise for many since the term ´Dry Eye´ seems to point to a primary lack of water. Many dedicated Dry Eye Specialists, however, have long realized that alterations of the lipid phase are often involved as indicated e.g. by foam on the tear film and lid margin from saponification of tear film lipids or lipid containing encrustations on the lid margin and around the base of eye lashes (collarettes).
Meibography was mainly a research lab technique during the 20th century
The ocular surface specialist is generally blessed compared to many other medial professions, in that most anatomical structures and pathological events in his interest can be easily seen.
In this respect the Meibomian Glands certainly represent an unexpected challenge because they are hidden in the depth of the tarsal plate inside the eye lids. From the front they cannot be seen through the anterior lid lamella with the skin and lid muscles. From the back of the lids through the relatively transparent conjunctiva the Meibomian Glands can be seen seen much better as whitish streaks of individual glands under suitable conditions, but this image does not reveal too many details (please see figure).
In a first wave of interest in the Meibomian Glands during the 1980s following the discovery of ´Meibomian Gland Dysfunction´(MGD) by KORB and HENRIQUEZ, a group around a man named James JESTER, performed early experiments that focused on hyper-keratinization of the gland epithelium. They visualized the glands by trans-illumination of the lids with infrared light from the frontal skin side and observation occurred from the back side through the conjunctiva. When such a visualization of Meibomian glands is only seen, it is termed ´Meiboscopy´and when the image is recorded it is termed ´Meibography´.
Non-contact Meibography with infrared illumination and CCD camera has greatly revolutionized clinical observation of the Meibomian gland
More recently a novel technique for Meibography was developed by Reiko ARITA and colleagues in Tokyo that is termed Non-Contact Infrared Meibography and was described in a seminal paper in 2008. This technique also:
uses infrared light because this appears to show the lipid content of the Meibomian Glands particularly well and it also
observes the glands from the conjunctival side, which certainly makes much sense, with an infrared digital camera attached to a slit-lamp.
this setting was custom-tailored by Topcon Japan Inc. and became later available to all interested clinicians as a commercial package.
In contrast to previous Meibography techniques the illumination is from the same side as the observation, i.e. from the posterior conjunctival side. Since relatively more light intensity reaches the Meibomian Glands the contrast of the image and thus the clarity is much better. ARITA and colleagues have meanwhile formed a Research Group termed the ´Lid and Meibomian Gland Working Group´(LIME, http://www.lime.jp/en/), they have made many advancements in the field of Meibomian Gland Dysfunction and also organize annual international research meetings.
The term non-contact refers to the fact that neither the lamp nor the camera is in contact with the eye - but since the eye lids must be everted in order to see the conjunctival surface some kind of device or the clinicians fingers must be in touch with the eye to perform the lid eversion.
A key finding in Meibography is the degree of gland drop-out
Meibomian Gland Drop-Out describes the disappearance of parts of the gland tissue in the Meibography observation which suggests a disappearance of functional gland tissue. This assumption appears correct as the degree of gland drop-out generally correlates with the gland function and with the degree of Dry Eye Disease.
Therefore Meibography this has become a valuable new diagnostic parameter in Dry Eye Diagnostics. The gland drop-out typically starts from the end of the Meibomian Glands, i.e. from that part which is away from the orifice on the posterior lid margin.
Apparently different pathogenetic influence factors may cause gland-drop because this is drastically increased in long-term contact lens wear, independent of the lens type, and gland drop-out also occurs in inflammatory conjunctival allergy as discussed in the chapter for Meibomian Gland Dysfunction (MGD).
Grading Scales are available for clinical use
Several semi-quantitative Grading Scales are available for Gland Drop-Out which basically all evaluate the relative amount of drop-out in different grades of differentiation.
A large number of visualization devices can nowadays display the Meibomian Glands and their drop-out including the class of so-called ´Topographers´ that are described in this chapter, and several more basic instruments that provide infrared imaging. Still, there is presently apparently no software available that can determine the exact degree of gland dropout fully automatic. The more basic devices just provide visualization and photography of the glands whereas more advanced systems often allow a manual tracing of the disappeared gland tissue that works with different degrees of exactness, particularly in potentially stressful clinical service situation.
Topographer Systems are typically more advanced. They usually provide more advanced illumination annd visualization techniques and a better image quality together with measurements and a structured documentation that can make the clinical daily life more effective and enjoyable.
Höchste Bild-Qualität bei der Meibographie ist möglich … aber sie benötigt eine spezielle Beleuchtungs- und Auswertungstechnik
Ein häufiges Problem bei der Darstellung der Meibomdrüsen im Augenlid des Patienten direkt in der Praxis des Arztes beruht darauf, dass Augenoberfläche eine natürliches ´Feuchtgebiet´ ist - eine Schleimhaut - und daher eine feuchte Oberfläche hat, die bei der Beleuchtung viele Reflexionen produziert.
Störende Reflexionen verschiedenen treten typischerweise auf den meisten Meibographiebildern auf und es erfordert einen gewissen Grad von Erfahrung des Untersuchers die Reflexionen möglichst gering zu halten um eine aussagekräftiges Foto für die klinische Verlaufs-Dokumentation anzufertigen.
Andererseits erlaubt es eine Fotodukumentation mit perfektem Kontrast und Auflösung die Meibomdrüsen so darzustellen, als wären sie freiiegend und nicht bedeckt von dem darüberliegenden Gewebe der Lidplatte und der Augenbindehaut. Dadurch ist die Struktur der Drüsen unmittelbar erkennbar für den Arzt … und auch für den Patienten.
Man darf annehmen, dass diese realistische Darstellung der Meibomdrüsen auch dem Patienten erlaubt unmittelbar zu verstehen, wie der Zustand ´seiner´ Meibomdrüsen mit dem Beschwerdebild des Trockenen Auges zusammenhängt und wie wichtig z.B. eine konsequente heimische Physikalische Lidrand Therapie für die Verbesserung der Erkrankung ist.
There is reason to assume that such immediate realistic visibility of the Meibomian glands will also increase the understanding and the care that is applied to these structure of utmost importance of ocular surface integrity.
Perfect and distortion-free imaging of such a difficult object requires sophisticated illumination and electronical image compensation systems that must be combined in order to achieve a perfect image. There is presently only one class of devices that can fulfill these standards and actually allow an unprecedented immaculate clarity in the imaging of Meibomian glands and their destruction which are the Lipiview and Lipiscan machines from TearScience.
As a (slight) disadvantage these machines are so specialized, that they are only optimized for Meibography (Lipiscan) or for Meibography and Lipid Layer Interferometry - they can thus not fully replace a multi-purpose work-horse like a topographer.
Advance illumination techniques allow imaging of the Meibomian glands in unprecedented clarity. Thereby the exact structure of normal Meibomian Glands and precise information on the their alteration in gland drop-out can be obtained. Images: Courtesy of TearScience Inc.