Deeper Insight - How can we TREAT Dry Eye ? ...
THERAPY 5 - ANTI-INFLAMMATORY THERAPY
... Some Insight into INFLAMMATION
NON-Steroidal Anti-inflammatory Drugs (NSAID)
STEROIDAL ... the cortisols
Specific Lymphocyte Activation Inhibitors
Adhesion-Molecule-Blocking (Lifitegrast)
UNCONVENTIONAL-Anti-Inflammatory-Therapeutics-
INFLAMMATION
The central amplifying factor in many vicious circles in Dry Eye Disease is a chronic inflammatory process inside the tissue that is progressively dysregulated and the tissue including that of glands is progressively destructed.
The observations that inflammatory events typically occur in Dry Eye Disease and the experience that chronic mucosal inflammation is a mighty amplifier of disease by self-perpetuating vicious circles with distinct worsening of the condition, has lead to the use of anti-inflammatory treatment.
Even when a chronic inflammation is assumed or diagnosed it makes sense to try to identify the primary problem that has lead to the eventual development of chronic inflammation ... in order to approach it by a suitable therapy option that tries to remove the primary causative factor instead of just dampening the secondary phenomenon of inflammation by very potent drugs ... that may also have potent side-effects.
A supportive therapy with tear supplements in addition to anti-inflammatory therapy is thus typically useful.
Severe Dry Eye Disease may need an at least temporary anti-inflammatory therapy approach in order to interrupt inflammatory vicious circles of disease reinforcement - when other therapies have failed - please see the sections on ´basic therapy considerations´ and on the concept for “staggered therapy“ of dry eye disease.
It may make some sense to consider whether severe Dry Eye Disease should preferably be treated in specialized centers where all diagnostic and therapeutic options are available.
HOW to ORGANIZE this TOPIC ???
When we think about practical routes for anti-inflammatory treatment in terms of concrete therapeutics
... we can either consider what is known best ... and thus comes easiest to our minds
... or we can dissect the pathophysiology of inflammation ... in order to look for therapeutic targets.
We will try to briefly follow both of these routes, where it applies.
First, it may be useful to ask ourselves ...
Inflammation is a very basic PROTECTIVE answer of tissues
to all kinds of pathogens
or to everything that is sensed as pathogens - by means of molecular characteristics (termed pathogen-associated molecular patterns, PAMP) that are sensed by respective receptors (pattern related receptors, PRR) as "Danger Signals" according the original "Danger Theory" by Polly MATZINGER and colleagues.
Such Danger signals are:
... of course microbial molecules such as LPS or microbial DNA etc. ...
... BUT also signals of ´something wrong here´ from the own tissues such as e.g. tissue wounding, cell activation, cell damage and extrusion of cytoplasmic constituents etc.
INFLAMMATION
INFLAMMATION is a very basic protective reaction in order to remove - devour and digest - the pathogen. To do so effectively, the integrity of the own tissue is temporarily neglected and partially corrupted ... for the higher aim to get rid of what is sensed as a ´pathogen´. Later the inflammatory reaction is followed by the induction of a repair of the tissue.
When the repair is chronically disturbed by (unnecessarily) ongoing (= chronic) inflammation, a chronic destruction of the functional tissue can occur. This results in a dominance of disorganized and thus useless connective tissue in the form of scarring, together with immature and not fully functional surface epithelium with a deficiency of mucins for water binding.
This is also the potential dramatic end stage of chronic long-term Dry Eye Disease that is described as "DEGENERATIVE TISSUE REMODELING and LOSS OF FUNCTION" - for more detailed information please see the section on ´How Dry Eye Disease gets WORSE´ and´Vicious Circles in Dry Eye Disease´.
ACUTE Inflammation - INFLAMMATORY MEDIATORS
ACUTE Inflammation is basically short-term for a few days and maintained by innate immune cells such as all types of phagocytic cells - first mainly granulocytes are active. The soluble factors that are used are small signaling molecules from several classes that all bind to respective receptors in order to produce an effect in target cells.
They have a primarily protective function but in unnecessary perpetuating chronic inflammation these inflammatory mediators lead to tissue destruction and then the signaling molecules as well as their receptors may become therapeutic targets.
Many different signaling molecules with a pro-inflammatory effect (= Inflammatory Mediators) are involved in inflammatory processes and modulate Inflammation. All signaling molecules act via binding to a respective receptor of a target cell. Inflammatory Cytokines are produced by many cells types and the same is true for inflammatory lipid mediators (eicosanoides) that encompass well known molecules such as different prostaglandins and leukotrienes - among other functions they induce pain. More restricted are vasoactive amines such as Histamine, Bradikinin and Serotonin that are produces by mast cells (mc in the diagram) and phagocytes (granuclocytes and macrophages - indicated by ´gr´and ´mo´in the diagram). An unstable and therefore short-time and short-distance acting mediator is the gas Nitric Oxide (No, blue-green in the diagram) that is produced mainly by macrophages and endothelial cells of blood vessels that induce relaxation of the peri-vascular smooth muscle cells and thus dilatation of the vessel with subsequent slow blood flow. Together with Histamine this promotes the inflammatory extravasation of plasma and cells into the tissue.
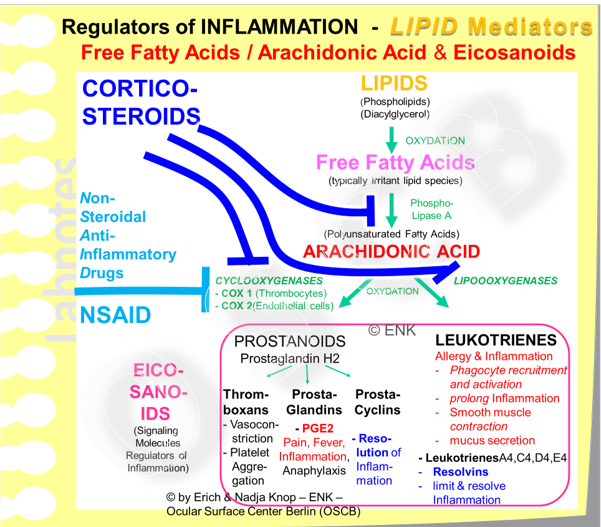
EICOSANOIDES are lipid mediators that derive from the lipid arachidonic acid. and encompass well known substances such as prostaglandins and leukotrienes. This is a free fatty acid that plays a role e.g in MGD because there bacterial lip0lytic enzymes were found to degrade lipids into free fatty acids that have several negative effects including stimulation of inflammation ... as reported by McCULLEY, SHINE, DOUGHERTY and coworkers - for more details please see the section of ´Overview on MGD´.
Eicosanoides other cells, e.g. phagocyte recruitment and induce pain
BIOGENIC AMINES are produced from Aminoacids and are released mainly by Mast Cells and also b Phagocytes (Macrophages and Granulocytes). They act vaso-active (such as histamine, bradykinin and serotonin) for the recruitment of blood components (cells and plasma with active factors) into the region of inflammation. This has the function to provide a more vigorous protective response by influx of plasma proteins (such as e.g. the complement system and antibodies) and by protective cells (leukocytes) as can be provided by the local protective environment of resident leukocytes.
Vaso-active Amines increase the permeability of the vessel walls with outflow of blood PLASMA, which consists mainly of water. This leads to the subsequent formation of edema with tissue swelling.
Inflammatory mediators alone and the subsequent edema stimulate nerve endings in the tissue and lead to pain.
INFLAMMATORY CYTOKINES are small signaling molecules that are produced by many cell types, not only by leukocytes, and they can have all different kinds of functions including growth, differentiation and regulation of cells and tissues. On subclass, the ´Inflammatory Cytokines´ are very effective promotors and mediators of inflammatory reactions. Some particularly important cytokines are Interleukin 1 (IL1) and interleukin 2 (IL2) because they promote the maturation of T-Lymphocytes. Therefore they are a prime target for very potent immuno-suppressive therapy.
NITRIC OXIDE (NO) is a potent signaling molecule that has some differences to the other molecules - because it is a gas and it is very short lived in the range of some seconds after production. Therefore it is mainly used as a signal for the producing cell itself (autocrine) or for cells in the immediate vicinity, which is termed paracrine. n the context of (acute) inflammation it is produced
by phagocytes to stimulate their own phagocytosis and particularly a more effective destruction of the swallowed substances, which may be microbes with certain resistance mechanism, and
by endothelial cells that induce the relaxation of the peri-vascular smooth muscle cells that leads to vasodilatation and promotes, together with the biogenic amines, the extravasation of blood components into the inflamed tissue.
As an early key event in Inflammation, blood components are recruited to the site in order to support the inflammatory attempt of clearing the tissue from a pathogenic impact. This occurs by influence on the endothelial cells of the vessel walls. Vaso-active amines increase the permeability of the vessel walls leading to outflow of PLASMA, which is mainly water, into the tissue with subsequent formation of EDEMA. Leukocytic protective CELLS from the vessels are also recruited by the help of adhesion molecules, that are expressed on the endothelium: in acute inflammation these are mainly phagocytic cells - in chronic inflammation they are mainly lymphatic cells that promote the progression into immune-mediated inflammation.
CHRONIC Inflammation occurs when the ´pathogen´ persists and provides continuous stimulation of the immune system.
This leads to in involvement of cells of the specific immune system - that is lymphocytes and their accessory cells for antigen-presentation. These cells are attracted by soluble mediators and by up-regulation of adhesion molecules on the endothelial cells of the vessel walls and on stromal cells and epithelial cells.
A Key Event in chronic MUCOSAL INFLAMMATION is the Recruitment of Leukocytes by Cell Adhesion Molecules (CAMs). Leukocytes that carry the Lymphocyte Function-Associated Antigen 1 (LFA-1) bind to vascular endothelial cells and also to cells in the tissue, e.g. epithelial cells, by InterCellular Adhesion Molecule 1 (ICAM-1). ICAM-1 is up-regulated in on the tissue cells in inflammation and makes them vulnerable to lymphocytes.
Chronic inflammation is a typical process in Dry Eye Disease
when a chronically low tear volume, decreased lubrication with increased friction and tear film instability with early break-up, hyper-evaporation and hyper-osmolarity
lead to chronic mechanical friction or hyper-osmolar stimuli
that induce an activation of the Ocular Surface Epithelium
An important factor in inflammation is the recruitment of Blood CELLS from the vascular compartment. This is promoted by the up-regulation of Adhesion Molecules on cells in the tissue and on the vascular endothelium inside the vessels. Thereby leukocytes in the blood with respective receptors can specifically emigrate at sites of inflammation out of the vessels and into the tissue in order to assist the protective process.
An important adhesion molecule that is up-regulated in inflammation is the intercellular adhesion molecule 1 (ICAM-1). It is an important modulator in inflammatory Ocular Surface Disease, such as Dry Eye Disease.
ICAM-1 on "tissue cells" binds to its cognate receptor, the Leukocyte Function-Associated Antigen 1 (LFA-1) on lymphocytes and other leukocytes. By the interaction of LFA-1 with ICAM-1 increased amounts of inflammatory cells can enter the tissue and bind there to tissue cells with later tissue destruction in chronic inflammatory Ocular Surface disease.
ICAM-1 is up-regulated in inflammatory Dry Eye Disease on "tissue cells" - these are vascular endothelial cells, stromal and epithelial cells in the tissue.
Antigen-Presentation - a critical step of Immune regulation - is also influenced by Adhesion molecules
The adhesion molecules ICAM-1 and its binding partner LFA-1 are also involved in the important process of antigen-presentation that initiates the specific immune answer. The adhesion molecules improve the mechanical binding between the antigen-presenting cell (APC) and the lymphocyte in the region where they interact by membrane-bound signaling molecules. This region is sometimes termed as the ´immunological synapse´ because of the similarities with the connection ofnerve cells. The interaction of ICAM-1 and LFA-1 is also though to provide ´co-stimulatory´ signals that promote a productive specific immune answer.
Some routes for Anti-Inflammatory treatment
Non-Steroidal Anti-Inflammatory Drugs (NSAID)
The first and ´oldest´ in the sense of most established drug with multiple effects - analgesic (relieves pain), anti-inflammatory, and anti-pyretic (relieves fewer) - is certainly Acetylsaclicylic acid (´Aspirin´ as it was termed by the first commercial manufacturer BAYER more than hundred years ago).
NSAID (middle left of the diagram) specifically block the cyclo-oxygenases (COX) enzymes that maintain the downstream metabolisation of inflammatory core substance Arachidonic Acid into the multitude of the, mainly but not exclusively, inflammatory Eicosanoids that encompass prostaglandins and leukotrienes.
Acetylsalicylic acid is a well known example of the Non-Steroidal Anti-Inflammatory Drugs (NSAID). NSAID are typically better pain-relievers than anti-inflammatory treatments. The mechanism of action is, that NSAID block the enzymes (Cyclooxygenases, COX) that perform the metabolism of the free fatty acid ARACHIDONIC ACID into the smaller but more potent lipid inflammatory signaling molecules known as eicosanoides (prostaglandins and leukotrienes - as shown in the diagram).
At the Ocular Surface, the topical application of NSAID is used since about the 1980s and their main indication is their analgesic and anti-inflammatory action after ocular surgery, mainly cataract surgery and refractive surgery. There are some reports over the years in the literature of cases of corneal melting after topical ophthalmic use of NSAID, which is certainly a very serious complication. The exact reason, whether such cases depended on the drug itself, or on other ingredients in the formulation or on predisposing factors of the patient, such as a hypersensitivity, never became quite clear. These events are widely known and have sharpened the attention of clinicians when topical ophthalmic NSAID are prescribed. Overall, ´in relation to the high frequency of post-surgical ophthalmic NSAID use, they have an impressive safety and efficacy profile´ as reviewed in 2007 by Mark ABELSON for the ´Review in Ophthalmology´. They certainly may have side-effects, just like any drug has, but this appears mainly due to inappropriate or over-use at the ocular surface.
NSAID are increasingly used in the therapy of Dry Eye Disease
For Dry Eye Disease, even though this is typically associated with unpleasant ocular sensations from irritation to often severe pain, topical NSAID were not always a typically used drug. In recent years however topical treatment of Dry Eye Disease with NSAID ophthalmic solutions has become more and more popular, because
NSAID represent an analgesic and sufficiently anti-inflammatory alternative to conventional anti-inflammatory drugs
with immediate effect, similar to corticosteroids,
but without the side-effects that corticosteroids have.
NSAID are used in moderate to severe Dry Eye in order to cover the lag time that specific lymphocyte activation blockers like ciclosporin need until they achieve a sufficient effect
... and is this lag time can typically take several weeks.
Popular Classes of NSAID are amphiphilic acids that resemble the basic structure of Acetylsalicylic Acid. They are based on e.g.::
ACETIC Acid, e.g. [Substance Name (Commercial Product, Supplier) ]
Bronfenac (Xibrom, Ista Inc.)
Diclofenac (Voltaren, Novartis Inc.; DifenStulln, PharmaStulln AG.; Dicloabak, TheaPharma S.A.)
Keratolac (Acular, Allergan Inc.; KetoVision, OnmiVision AG)
Nepafenac (Ilevro, Alcon Inc.; Nevanac, Alcon Inc.)
INDOLacetic Acid
Indometacin (Indophthal, Bausch+Lomb Inc.)
PROPIONIC Acid
Flurbiprofen (Ocufen, Allergan Inc.)
Pranoprofen (Santen Pharmaceutical Inc.)
Generally IMMUNO-SUPPRESSIVE
Corticosteroids
The source of Glucocorticoids and their precursors is the Adrenal Gland from where they are distributed via the blood stream throughout the body. The Adrenal Gland is seen here in the diagram in the bottom middle over the ´ovary´.
When we think of anti-inflammatory/ anti-phlogistic therapy - well established therapeutics such as cortisol derivatives - corticosteroids - come to our mind. These are steroid molecules, that derive from the lipid cholesterol by metabolization in the cortex of the adrenal gland - similar to the steroidal sex hormones.
They are probably one of the oldest established therapeutics that very specifically act anti-inflammatory, are usually very reliable and a large body of experience exist.
Glucocorticoids are mighty own hormones of the body for the maintenance of chronic stress. Therefore they are involved in many different processes and they also block almost all steps of inflammation very effectively. Due to their pleiotropic action on many systems the also have many potent side-effects even in topical use at the ocular surface, particularly when given ´too long ... and too much´.
The experience with corticosteroids, however, also tells us that they are not only very potent drugs but they also have very potent side effects. Apart from systemic side effects they may cause locally in the ocular region a well known risk for the development of glaucoma and cataract. Therefore they should only be used short term ... and typically very effectively block/ stop inflammation. Another description of their mode of action is that corticosteroids ... "bring inflammation to full completion". Whatever this specifically means... practically they stop inflammation relatively quickly.
Corticosteroids basically act against all steps of the inflammatory cascade from the activation of innate, e.g. phagocytic cells, over the formation of inflammatory mediators to the activation of lymphatic cells and modulation of the immune reaction. So, corticosteroids are definitely a wonder drug ... BUT, since they are the most important hormones of the body for the maintenance of chronic stress. they are mighty regulators that influence many systems and therefore they have many severe sides effects - if used inappropriately, which is, in a very simplified way, too long and too much.
CORTICOSTEROIDS:
potent anti-inflammatory against all events of inflammation
different metabolites have different potency
immediate effect
severe side effects, also in topical ophthalmic use (e.g. cataract, glaucoma)
Specific Lymphocyte ACTIVATION INHIBITORS
Lymphocyte activation typically occurs in relation to the process of antigen-presentation. This occurs typically by a professional antigen-presenting cell (APC), such as dendritic cells (with have typical dendriform cytoplasmic extensions), by macrophages of B-Lymphocytes.
Potential anti-inflammatory therapeutical targets are basically all players that are involved in Antigen-Presentation and Lymphocyte Activation.
Many of the immune factors of peculiar numbered names that start with the letters "CD". This refers to Cluster of Differentiation and refers to a specific nomenclature whit ever increasing numbers the new molecules are discovered. Many of these molecular factors also have ´Real´ or at least slightly better understandable names such as the ICAM-1 (an acronym for ´InterCellular Adhesion Molecule 1´) ... which is CD54.
Some Molecules of Interest for Antigen-Presentation and Lymphocyte Activation
The diagram shows molecules that are important for antigen-presentation and lymphocyte activation and are thus promising targets for anti-inflammatory Presently used, and highly effective, drugs at the ocular surface typically block the synthesis of two important interleukins (soluble signaling molecules abbreviated by IL and a number) for lymphocyte activation (IL-1 and IL-2). Lifitegrast is using another target in the form of blocking the interaction of adhesion molecules. Apart from many other functions in inflammation, these also assist in antigen-presentation by mechanically linking the respective cells - please see below for ´Lifitegrast´.
Foreign antigens are presented on the MHC-class II molecule
in chronic inflammatory disease, also aberrant antigen-presentation can possibly occur by cells that have up-regulated the antigen-presentation molecule MHC-class II. This also occurs in ocular surface epithelial cells in Dry Eye Disease and can potentially lead to the presentation of auto-antigens of the epithelium ... with a potential risk for auto-immune inflammation.
the T-cell-Receptor (TCR) on T-Lymphocytes identifies cognate antigens on MHC-class II
CD3 is an accessory molecule, that the TCR needs for full function
CO-Stimulatory Molecules are further accessory molecules that are needed for a productive immune answer
CD80 and CD86 on T-cells and their binding partner
CD28
Cytokines, soluble signaling molecules, are also important, because they promote the activation of lymphoid cells.
IL-1 is used, e.g., by Antigen-presenting cells to stimulate/ activate T-Lymphocytes during antigen-presentation
IL-2 is produced for Self-Stimulation, by activated T-Cells to promote their maturation
Specific Cytokine receptors to which the cytokines bind and that produce the effect by intracellular signaling within the lymphocyte.
So by now, we have a nice collection of molecules (all shown in the adjacent figure) that are necessary for lymphocyte activation - thus they are also promising targets for potential anti-inflammatory therapeutics that are indicated in blue.
Cyclosporine A / CICLOSPORIN A (CsA) Ophthalmic Solution
Cyclosporine is a very potent immunosuppressive drug, that was approved in the end 1970s for suppression of tissue rejection after solid organ, e.g. kidney, transplantation.
It blocks an enzyme (calcineurin) that is necessary for the synthesis of the cytokine signaling factor Interleukin 2 (IL-2) that promotes lymphocyte maturation. Cyclosporine A has less side-effects at the same efficacy compared as compared to corticosteroids, when given systemically, and can therefore be used long-term.
At the ocular surface is is however used topically and in a very low dose (0,05%) so that systemic side effects can be reasonably excluded. It was FDA approved in 2003 for topical use in inflammatory moderate to severe Dry Eye Disease in the human. It is effective in chronic Dry Eye Disease because it dampens the immune modulated aspect of the inflammatory pathways that typically occur in advance stages of Dry Eye Disease.
Since the FDA approval many studies have been performed on the Êfficacy and Safety of Ttopical Cyclosporine Eye Drops. It appears as the only FDA approved treatment that may lead to an (re-) increase of own aqueous tear production in patients with chronic dry eye.
Since Cyclosporine is a very specific lymphocyte activation blocker without a direct effect as a secretagogue on glandular tissue, the observed effect on tear stimulation may be attributed to a release of the impairment in afferent sensory innervation that is the main concept for aqueous tear deficiency in chronic inflammatory Dry Eye. Therefore, the potential positive effect on secretion can be regarded as evidence for the validity of the present concept of afferent sensory impairment as a reason for lacrimal gland dysfunction (LGD).
CYCLOSPORINE:
potent specific anti-inflammatory drug(Lymphocyte activation blocker)
long lag phase until effect is achieved (typically several week until full effect)
no known side effects in topical ophthalmic use of 0,05% emulsion
except for mild local irritation that is conceivably due to the oily formulation
LIFITEGRAST (LFA-1 Adhesion-Molecule Blocking)
Recently FDA-approved is a small molecules that binds to a cell adhesion molecule - the Lymphocyte Adhesion Molecule LFA-1 - and thus blocks the interaction/ binding with its main binding partner - the Inter-Cellular Adhesion Molecule 1 (ICAM-1). This small blocking molecule is termed (Lifitegrast (available as Xiidra for Dry Eye Disease from SHIRE Inc.). It blocks the interaction with ICAM-1 on tissue cells and vascular endothelial cells and can thus decrease the immigration of inflammatory cells into the tissue and the damage they do to the tissue when immigrated. This is a promising new approach in inflammatory Dry Eye Disease and a valuable addition to the use of the lymphocyte activation blocker Cyclosporin A (CsA).
The interaction of the Cell Adhesion Molecules ICAM-1 on tissue cells and its partner LFA-1 on leukocytic immune cells is a central regulatory and promoting mechanism in the inflammatory pathways in moderated to severe Dry Eye Disease. The blocking of this interaction by a small blocking molecule (Lifitegrast), that is small enough to be applied topically, thus appears as a promising new therapeutic route to treat ocular surface disease.
Lifitegrast binds to an important adhesion molecule (Lymphocyte Adhesion Molecule LFA-1) on lymphatic cells and other leukocytes. Leukocytes use LFA-1 during their migration through the vascular system of the body (termed recirculation) in order to detect tissue regions where inflammatory events occur and ´help´ from professional immune cells is needed by the ordinary tissue cells in order to clear what is sensed as a pathogen.
In inflamed tissues the endothelial wall cells of the smaller blood vessels are activated to up-regulate adhesion molecules such ICAM-1. It acts like a door steward who attracts by-passing leukocytes (carrying a suitable surface binding molecule, such as LFA-1) to ´come in´ to the tissue. The binding between lymphocytes and vessel wall slows the traveling lymphocyte down and allows it to ´emigrate´ from the vessel and to ´immigrate´ into the tissue. The interaction of the adhesion molecules is at the same time some kind of passport control.
In inflamed ocular surface tissues in moderate to severe Dry Eye Disease, not only the endothelium but also other tissue cells such as e.g. fibrocytes, antigen-presenting dendritic cells, and epithelial cells up-regulate ICAM-1. ICAM-1 is apart from immigration of lymphocytes also involved in the process of antigen-presentation and in binding to the epithelial cells. Binding to stromal and epithelial cells promotes contact and thus promotes tissue destruction. The adhesion molecule ICAM-1 and its binding partner LFA-1 therefore ´sit´ in a central position of the inflammatory pathways in the Ocular Surface(and other) tissues. The blocking of their interaction thus appears as a major step forwards in fighting Ocular Surface inflammation by a specific therapy.
LIFITEGRAST:
specific anti-inflammatory (adhesion molecules. LFA-1, blocker)
long lag phase until effect is achieved (typically several week until full effect)
no known side effects in topical ophthalmic use, except for mild local irritation
BIOLOGICALS
´Biologicals´ are therapeutic substances that resemble natural molecules of the body or are even such ´own´ substances. Their use is not new because also hormones that are applied in a therapeutical function all under this category, such as insulin or growth hormone, pancreatic enzymes etc. The ´modern´ biological are often ANTIBODIES against important factors or their receptors in disease, such as ANTI-Vascular endothelial growth factor.
There are, however, not only antibodies but a small proteins that bind by protein-protein interactions to their molecular targets. When these targets are important molecules in the inflammatory pathways such molecules practically provide ´anti-inflammatory´ therapy.
Unconventional Anti-Inflammatory Therapeutics & LIPID MODULATION
AZITHROMYCIN
AZITHROMYCIN is a macrolide antibiotic that acts, after topical application onto the lid and into the conjunctival sac within short-term of a few days. It has a high tissue storage, mainly in phagocytic cells. The phagocytes thereby bring it to sites of inflammation and the dosage can be reduced to twice daily over a few days ... which will certainly increase the compliance of patients. Its use at the ocular surface is relatively recent but promising.
Topical AZITHROMYCIN, a macrolide antibiotic that was originally developed for infectious ocular surface disease, appears to have if fact multiple favorable effects in Meibomian Gland Dysfunction (MGD). According to literature reports, has: (1) an antibiotic effect against the overgrowth of the commensal lid bacteria, (2) it blocks the breakdown of irritant lipids into potent inflammatory free fatty acids, and (3) it has a stimulating effect on the secretory cells (Meibocytes) of the Meibomian Gland.
Interestingly Azithromicin, according to many studies, also has an anti-inflammatory effect, that is multi-factorial. It negatively interferes e.g with events upstream and downstream of arachidonic acid. This is one of the irritant free fatty acids that are produced from the normal Meibomian lipids by bacterial enzymes. Arachidonic acid is the origin of metabolism into as cascade of potent inflammatory signaling molecules, termed eicosanoides. Eicosanoides are potent modulators/ amplifiers of acute inflammation and cause pain. Azithromycin also has other immune-modulatory/ immune-suppressive functions on immune phagocytic cells, where they inhibit the production of inflammatory cytokines and chemokines and on epithelial cells.
Another tempting (side-) effect of Azithromycin is, that it apparently promotes the lipogenesis in Meibomian Gland secretory cells (Meibocytes) as was reported by the group of David SULLIVAN and colleagues in cell culture experiments with immortalized Meibocytes.
Azithromycin has an anti-inflammatory effect via several pathways. It limits the metabolism of inflammatory lipid species upstream of the crucial molecule Arachidonic Acid, which leads to its decreased production, and it also inhibits its downstream metabolisation into all the inflammatory Eicosanoids. Further effects concern e.g. an inhibition of inflammatory cytokine and chemokine production by phagocytes.
This would make Azithromycin an almost ideal drug for the treatment of MGD, because everything that is needed would by available in just one drug:
(1) anti-biotic action that dampens the protein synthesis and thus growth and replication of the apparent overgrowth of commensal bacterial species on the lid margin and conceivably inside the Meibomian glands
(2) anti-inflammatory action e.g. by an inhibition of the production of arachidonic acid and pro-inflammatory eicosanoides and by inhibition of the production of inflammatory mediators by phagocytic cells
(3) lipogenic action as a promoter of lipid synthesis in secretory Meibocytes, that could be advantageous in the altered Meibocytes in the lipid deficient condition of Meibomian Gland Dysfunction (MGD)
Some kind of disadvantage, however is, that Azithromycin is approved as a therapy against inflammatory conjunctivitis. Therefore its use in MGD is possible ... but off-label.
AZITHROMYCIN:
antibiotic drug (macrolide) with broad spectrum, approved for infectious conjunctivitis
important secondary effects:
anti-inflammatory
promotes lipogenesis in cell culture
quick effect within some days, long tissue storage - therefore short application period
no known side effects in topical ophthalmic use, except for mild local irritation
LIPID MODULATION
TETRACYCLINES
Systemic Tetracyclines and their derivatives, e.g. Doxycycline and Minocycline, represent an established therapy option for moderate to severe cases of blepharitis and obstructive MGD.
The mode of action is not so much an antibiotic one because they are typically given in a dosage that is below the antibiotic threshold. Tetracyclines instead inhibit the bacterial enzymes (lipases) that degrade the physiological Meibomian lipids and lead to the formation of irritant free lipid species.
The effect on lipid normalization is relatively reliable but has a long lag phase and typically takes several weeks up to a few months for full effect. The use of tetracyclines in moderate to severe cases of MGD and blepharitis therefore requires a high compliance of the patient which is often best provided by good information on his condition and the expected long-term course of improvement in sign and symptoms.
Tetracylines, at least in systemic application as necessary for the described therapy of MGD and blepharitis, have severe and well known side effects. These depend mainly on their strong calcium binding and thus concern issues with formation and differentiation of bones and teeth - they can lead e.g. to development of dark bands in teeth due to a deposition inside the matrix of developing teeth. This results in a strong contra-indication of tetracyclines during pregnancy, breast-feeding and childhood. Further side-effects include a photosensitization of the skin, potential oto-toxicity on the sensory cells of the inner ear cochlea, hepato-toxicity etc.
When long-term systemic use of tetracyclines, as described here, is considered it is thus necessary to weight the pros and cons of therapy in view of the patient´s systemic health condition.
TETRACYCLINES:
broad spectrum antibiotic
however, in moderate to severe MGD and blepharitis the blocking of bacterial lipid degrading enzymes by sub-antibiotic doses with long-term application is intended for lipid.normalization
long lag phase (several week to some months)
often effective
broad spectrum of potential severe side-effects require a qualified considerations of pros and cons