Deeper Insight into ... DIAGNOSIS 2 -
SECRETION / PRODUCTION of Tear Components
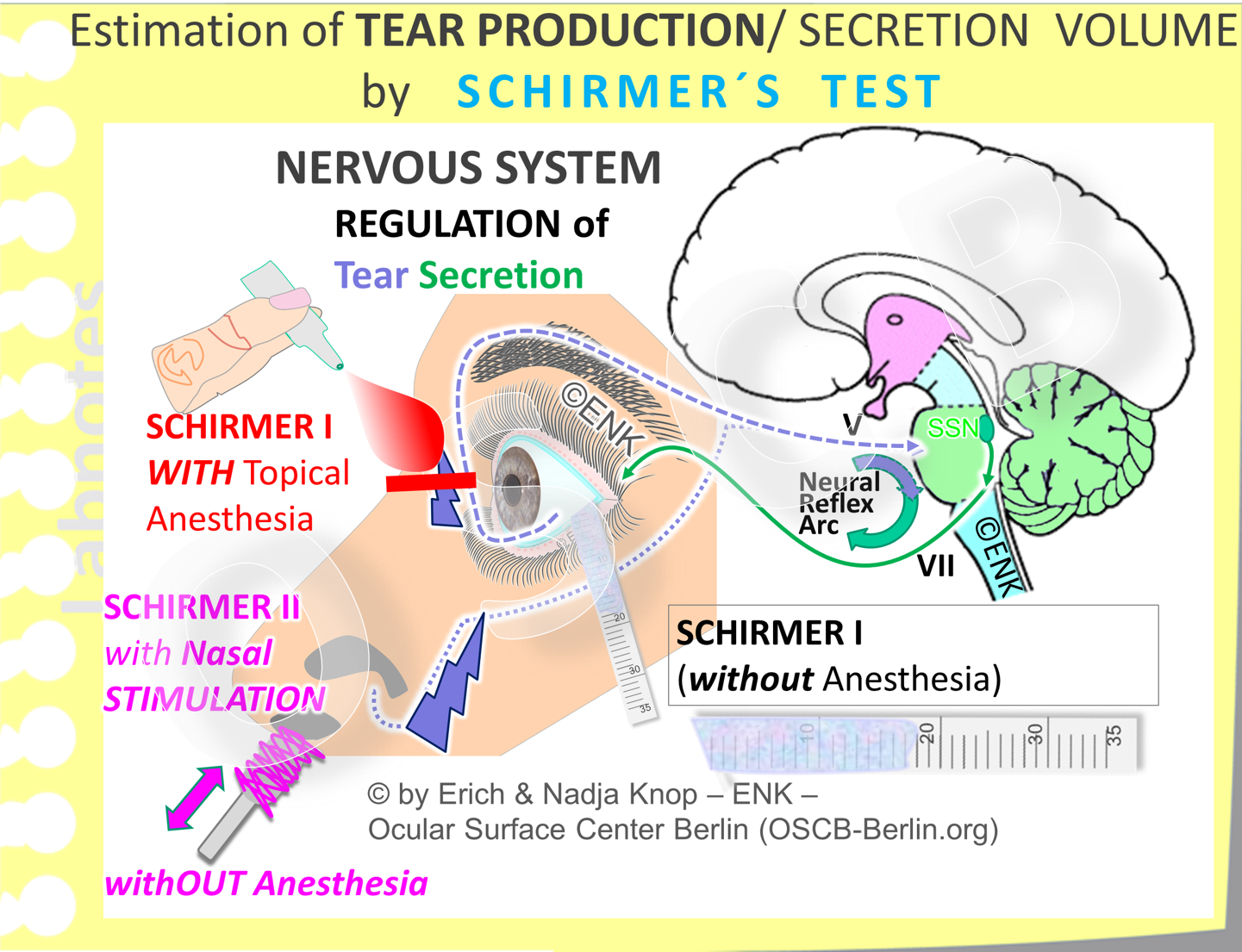
AQUEOUS Tear SECRETION (SCHIRMER´S Test)
SCHIRMER´s Test is probably the oldest and most established test for tear analysis. It was developed by Otto SCHIRMER in the early 20th century (1903). Several variations of this test have been developed, e.g. with or without prior topical anesthesia, or with additional nasal mucosal stimulation of tear flow, and with the eye lids open or closed or with different positions of the cornea, e.g. upward gaze vs. straight.
Schirmer I (without anesthesia)
The aqueous lacrimal SECRETION volume is measured by SCHIRMER´s Test that collects the tears on a strip of filter paper, hanged over the lower temporal lid margin, during a period of 5 minutes . The ocular surface and the lacrimal glands are connected by a neural reflex arc for secretory regulation. It consists of the afferent sensory (blue interrupted line) and the efferent secreto-motor green solid line) nerves - together with the regulating brain stem including the efferent superior salivary nucleus (SSN dark green). There are different variations of the original test that either add a topical anesthesia or, instead, add a nasal mucosal stimulation.
The most frequently used version about which most data exists, is the original version without anesthesia. When a cut-off value of 5,5 millimeter of wetting is used, in order to differentiate between normal, i.e. more tears, and pathological in the sense of Dry Eye Disease, i.e. less than 5,5mm of wetted strip length the test is relatively precise. With this cut-off value its sensitivity, as defined by the ability to identify true positive Dry Eye Patients, is 85% and its specificity, defined as avoiding false positives is 83%, i.e. only 17% of identified individuals with such a low secretion rate do not have a Dry Eye Pathology.
The most frequently used version about which most data exists, is the original version without anesthesia. When a cut-off value of 5,5 millimeter of wetting is used, in order to differentiate between normal, i.e. more tears, and pathological in the sense of Dry Eye Disease, i.e. less than 5,5mm of wetted strip length the test is relatively precise. With this cut-off value its sensitivity, as defined by the ability to identify true positive Dry Eye Patients, is 85% and its specificity, defined as avoiding false positives is 83%, i.e. only 17% of identified individuals with such a low secretion rate do not have a Dry Eye Pathology.
WORKING PRINCIPLE:
The original simple Schirmer test (termed SCHIRMER 1) collects the tears that are secreted during 5 minutes without anesthesia.
The original simple Schirmer test (termed SCHIRMER 1) collects the tears that are secreted during 5 minutes without anesthesia.
A standardized strip of filter paper is hanged over the temporal third of the lid margin. One reason for this position may be that this is close to the entrance of the lacrimal gland excretory ducts into the conjunctival sac. Another reason not to hang the paper strip in the middle of the lid margin is that the rough filter paper could hurt the corneal surface upon lid closure.
Then the eye is closed for five minutes. Schirmer´s test measures the aqueous secretion by collecting the produced tear fluid on the ocular surface in a strip the filter paper over the time of 5 minutes. The filter paper is typically commercially available readily cut paper strips or Whatman Paper No.1 or lackmus paper. The latter makes the wetted zone better detectable even after the tears have dried. This is particularly useful when the dried Schirmer´s strip is later archived in the patients files.
The surrogate parameter for the aqueous tear volume that is secreted during over 5min is measured in millimeters of wetting on the paper strip. Since all aqueous fluid is soaked up, the measurement will reflect the total aqueous secretion that derives from the lacrimal gland including that of the accessory lacrimal glands adjacent to the conjunctiva.
RESULT
Since the very sensitive ocular surface including the lid margin is irritated during the insertion of the rough filter paper strip, the SCHIRMER I Test without anesthesia measures some kind of a stimulated aqueous secretion.and therefore gives some indication of the secretory capacity and thus of the health of the lacrimal glands.
Schirmer I (With AnestheSia )
When topical anethesia is used this blocks all stimulation that may be exerted by the toughing the bulbar surface of eye lids and transforms the Schirmer test into a test for BASAL Sectetion. This is termed SCHIRMER 1 Test with anesthesia.
A variation of the test is sometimes preferred in which the ocular surface is topically anesthetized some minutes, typically 5min, before insertion of the filter strip.
This makes the whole procedure better tolerable for many patients because the rough filter paper can be quite irritative.
This variation with topical anesthesia is termed SCHIRMER Test I with anestheisia ... and comes closer to some kind of a basal secretion rate.
However this test does not seem to correlate very well with the secretory capacity of the lacrimal glands and thus health of the lacrimal glands. It does therefore not correlate very strongly with ocular surface damage in Dry Eye Disease.
Schirmer´S Test with Nasal STIMULATION) ... (Schirmer 2)
SCHIRMER 1 Test with nasal stimulation (= SCHIRMER 2) is a modification of the simple Schirmer 1 test (without anesthesia) in which the nasal mucosa is stimulated by a cotton swab during the full time (5min) of the test. This test is useful when the ordinary Schirmer 1 test has revealed a borderline low score. It is performed in order to test the maximal stimulated capacity of aqueous secretion. The results of this test show the best correlation with ocular surface damage as seen upon Rose Bengal staining.
SCHIRMER 2: The SCHIRMER 1 Test with nasal stimulation is a modification of the simple Schirmer 1 test (without anesthesia) in which the nasal mucosa is stimulated by a cotton swab during the full time (5min) of the test. This test is useful when the ordinary Schirmer 1 test has revealed a borderline low score. It is performed in order to test the maximal stimulated capacity of aqueous secretion. The results of this test show the best correlation with ocular surface damage as seen upon Rose Bengal staining.
Another interesting and important variation of Schirmer´s test is the application of stimulation of the nasal mucosa at the inside of the nose) that was proposed by Kazuo TSUBOTA in the early 1990s. The rationale for nasal stimulation is that the sensory fibers converge to the brain stem by the same pathway (cranial nerve V, Trigeminal) as the ocular surface fibers. Nasal stimulation thus increases not only the secretion of the nasal glands by the efferent secreto-motor nerve (cranial nerve VII, Facial) but by the same nerve it cross-stimulates also the lacrimal and accessory lacrimal glands. The reason is, that the origin for secretion of the whole facial glands, with exception of the ear salivatory gland, comes from the same command center in the brain stem (the superior salivatory nucleus- ´SSN´ in the diagram).
The NASAL STIMULATION tear secretion test is performed WITHOUT anesthesia, like the original Schirmer´s test and is sometimes termed Schirmer 2 Test.
Nasal stimulation increases the aqueous secretion strongly by about 50%. This can be assumed from the finding that experimental nasal anesthesia that blocks the stimulatory effect brings the increased secretion rate down by one third as reported by Steven PFLUGFELDER´s group. It may thus be assumed that the strong irritation that apparently occurs due to nasal mucosal stimulation represents a maximal secretory stimulation for the lacrimal glands and can thus reveal the maximal secretory capacity and ´health status´ of the lacrimal glands.
This would explain, why this test has the highest correlation with ocular surface damage shown by Rose Bengal staining as reported by TSUBOTA in another study on the importance of reflex tearing in 1999. Schirmers test with nasal stimulation thus appears to reflect the functional status of the lacrimal gland more correctly than conventional Schirmer tests.
In line with this, Schirmer´s test with nasal stimulation in fact shows that patients with Sjögren´s syndrome Dry Eye Disease have a decreased score as compared to Non-Sjögren Dry Eye patients as reported by FUJISAWA and colleagues. These results fit well with the pathogenesis of chronic auto-immune inflammation in Sjögren´s syndrome that destroys the lacrimal gland tissue and thus the effective secretory capacity.
LIPID DELIVERY - DIAGNOSTIC EXPRESSION of the MEIBOMIAN GLANDS
DIAGNOSTIC EXPRESSION Test. At a normal appearing lid margin (top images) it is not immediately clear whether the Meibomian Glands are functional or not. Functional means whether clear liquid oil can be delivered through an open orifice onto the lid margin with the mild pressure that occurs during a blink, since these holocrine glands are anyway continuously secreting lipids. The testing for patency of the gland orifices is thus the aim of the DIAGNOSTIC EXPRESSION Test. When mild pressure is applied onto the lid margin from the skin side - simply with a finger (middle image) or with a special standardized instrument (Meibomian Gland Evaluator, MGE, TearSeience Inc - lower two images) a normal gland will ´deliver´ clear oil as a little puddle onto the lid margin around the orifice (middle figure). An obstructed gland (MGD) in contrast will not deliver any lipids upon mild diagnostic expression.
The simplest test for the effective functionality of the Meibomian glands is the DIAGNOSTIC Gland Expression. This is a test for the DELIVERY of already secreted Oil from the Meibomian Gland ducts onto the posterior lid margin.
It is somewhat like the ´oily equivalent´ of Schirmer´s Test in the respect, that
- it is testing secretion onto the ocular surface - which in case of the Meibomian Glands is more equivalent to the actual delivery of the lipid phase -
- from the respective glands - in this case the holocrine Meibomian Glands.
There are, however, differences to Schirmer´s test because Diagnostic Expression
- does not test the volume of secretum
- but it tests
- whether the orifice is open and thus the secretum will flow freely once there is just a mild pressure
- or whether the orifice is blocked and thus a case of Non-Obvious MGD (NOMGD => pleases see there for details) is present in these glands.
Diagnostic Expression uses very mild pressure for diagnostic gland evaluation and is not to be confused with therapeutic hard expression
It is termed Diagnostic Expression of Lipids and performed by a very mild pressure from the skin side onto the anterior lid border in order to check if normal clear liquid Meibomian oil is readily delivered by the Meibomian Glands and thus available in the duct to be released onto the lid margin by the mild pressure that occurs during the normal blink movement of the eye lids.
Such a mild pressure in the range of normal lid pressure amounts to 1,25 g/cm2, as detailed by the developer of this test (Donald KORB, Boston, MA) . This can be exerted simply by a very mild finger pressure. For standardization it would of course be preferable to use to a standardized pressure applicator - the Meibomian Gland Evaluator (MGE) that is available from TearScience Inc. This is a very simple and inexpensive instrument but helps to make sure that this important diagnostic technique as always performed in an exact and reproducible way.
Standardization of pressure is preferred for a standardization of test results
A standardized low pressure is preferable
- in order to avoid high pressure onto the lid and thus also onto the eye ball which can have detrimental effects on the eye.
- because the intended Diagnostic Expression must remain clearly different from a Therapeutic Expression of the Meibomian Glands that has the intention to empty obstructed glands. Even though the therapeutic expression typically needs much higher pressure, a diagnostic expression will gradually transform into a therapeutic one when the applied pressure becomes too high.