Deeper Insight - How can we TREAT Dry Eye ? ...
THERAPY 3 - MANAGEMENT of Tear DEFICIENCY => Tear SUPPLEMENTATION
Some Insight into TEAR DEFICIENCY
Three Types of Tear Film Deficiency
LIPID Deficiency is most frequent
Therapeutic MANAGEMENT of Tear-FLUID in Dry Eye Disease
Tear STIMULATION - Secretagogues
Tear SUPPLEMENTATION - Eye Drops or Spray
Tear RETENTION - Punctum Plugs
SPECIFIC Tear SUPPLEMENTATION
Tear Supplements should be FREE of PRESERVATIVES
LIPID SUPPLEMENTATION
AQUEOUS SUPPLEMENTATION - incl. Hyaluronic Acid
MUCIN DEFICIENCY & Supplementation
SECRETAGOGUES - Stimulators of Secretion
TEAR FILM DEFICIENCY due to Gland Dysfunction is a Prime Pathology in Dry Eye Disease
... together with the inability to FORM a Tear FILM from the available tear fluid, which members of the Ocular Surface Center Berlin (OSCB) have termed as Eye ´Lid and Blinking Deficiency´ (LBD).
A Deficiency of the tear film with respect to the lack of at least one specific tear component is the most frequent problem in patients with Dry Eye Symptoms and Disease.
The tears - the vehicle to maintain the essential pre-condition of MOISTURE at the ocular surface - consist of three different classes of substances that are related to the three layers which typically form an intact tear film.
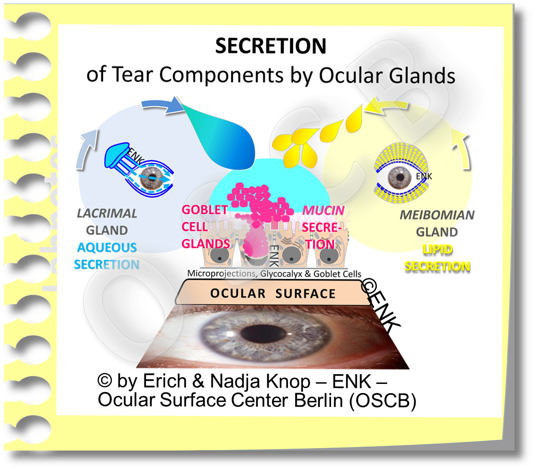
The three DIFFERENT TEAR COMPONENTS are:
WATER
(with many biologically active proteins)
LIPIDS
MUCINS
They are PRODUCED by three DIFFERENT Types of Ocular GLANDS:
LACRIMAL and ACCESSORY Lacrimal Glands
MEIBOMIAN Glands
GOBLET CELL Mucin Glands
Tear components have DIFFERENT FUNCTIONS:
the AQUEOUS Phase
appears to be the main phase not only by volume but also by inherent ´originary´ effect for regulating and maintaining the integrity of the mucosal tissue
because it has the necessary water for moisture and also a plethora of solved active ingredients of any kind - please see the section on tears & tear film.
but the aqueous phase can probably do almost nothing without the assistance of the other phases ... because...
the MUCIN Phase appears necessary, according to early investigations by Frank HOLLY and Mike LEMP, to allow binding of the aqueous to the epithelial surface as a more or less homogeneous layer-like structure... which we then regard as wetting, instead of just forming isolated drops as seen in the ´banner´ image for the section of tears and tear film.
the LIPID Phase serves in many aspects for the stability of the tear film. The main effect is thought to be its retardation of the evaporation rate of the aqueous phase that preserves the necessary volume of tears on the surface. In addition it may also function to aid in spreading of the tears into a sufficiently homogeneous film with a sufficiently thin width and a sufficiently smooth surface.
SO, ... NOW ... with this in mind if becomes obvious, THAT and WHY there are also at least THREE DIFFERENT TYPES of Tear Film DEFICIENCY
... and from here it is not far to realize that the approach in Tear Supplementation can typically not be ´one fits or all´.
... which in return may suggest, that an exact tear film diagnosis is necessary, to find out which component of the tears is primarily missing ... and thus needs to be supplemented in therapy
Two different types of Dry Eye are more frequent - with different pathophysiology and different therapy requirements
According to an early precise investigation in clinical practice, of the different types of Tear Film Deficiency that occur in Wetting Deficiencies with respect to Dry Eye Disease, performed by Heiligenhaus, Koch, Kemper, Kruse and Waubke: the two most frequent types of wetting deficiencies are primary due to
There are at least two main types of Dry Eye that both lead to a low tear volume but have a different pathophysiology background and thus different therapeutical approaches.
LIPID Deficiency - which occurred in 76,7% of patients
... is MOST FREQUENT
later studies that specifically investigated MGD, which is the reason for lipid deficiency, revealed even higher prevalences of up to 87%
AQUEOUS Deficiency - which occurred in 11,1% of patients ... whereas a primary
Mucin Deficiency was ONLY observed in a distinct minority of 4,4% of patients.
These about 5% of patients who have a primary mucin deficiency also answer the frequent question where the missing 5% come from, when the two frequencies for lipid and aqueous deficiency are summed up !
These results have basically proven to be in accordance with later studies, e.g. on Lipid deficiency due to MGD in Dry Eye patients by Jun SHIMAZAKI and colleagues and by Jutta HORWATH-WINTER and colleagues and by several other studies afterwards.
We can thus safely assume, that LIPID and AQUEOUS Deficiency are the two most frequent single deficiencies of Tear Film Components - among which LIPID-Deficiency represents BY FAR the MOST FREQUENT PRIMARY Type of Tear Deficiency.
"PRIMARY" tear deficiency in this context means, that it is the first or main factor in a Wetting Deficiency. However, this does not preclude that other types of tear film deficiency can later occur that show deficiency of different tear factors together in a mixed form:
A respective occurrence of "Mixed Types" ofTear Film Deficiency in Moderate to Severe Dry Eye Disease has been reported by Mike LEMP and Tony BRON
The Pathology in Dry Eye Disease has an inherent tendency to become worse since it is driven by amplifying factors like Vicious Circles and Inflammatory Processes - which is clearly shown in the HOLISTIC DYNAMIC CONCEPT on Dry Eye Disease of the OSCB.
Moderate to Severe Dry Eye Disease due to a primary lipid deficiency will, with ongoing duration of the condition and with consequent increasing destruction of the surface tissue and increasing impairment of more and more physiological functions, eventually also impair the aqueous secretion of the lacrimal gland.
This can happen, according to the present concepts, either indirectly by impairment of the sensory limb of the neural reflex arc for tear secretion or by the action of inflammatory mediators and cells.
The Tear Film is the most important (functional) part of the Ocular Surface
The BASIC CAUSATIVE FACTORS for Dry Eye Disease are a Deficiency of Tear SECRETION and/or of Tear FILM FORMATION because this impairs to keep the ocular surface moist everywhere &every-time and impair perfect visual acuity.
The tear film is certainly the most important functional part of the Ocular Surface for the maintenance of Ocular Surface INTEGRITY and for the VISUAL FUNCTION as explained in the chapter for ´Ocular Surface´ of this webpage.
The Ocular Surface has two Main Functional Complexes, which are Tear Secretion and Tear Film Formation, that pave the way for this.
Consequently, a failure of these functional complexes leads to the BASIC CAUSATIVE FACTORS for Dry Eye Disease which are a DEFICIENCY of Tear SECRETION and/or a Deficiency of Tear FILM FORMATION because this impairs to keep the ocular surface moist everywhere & every-time and impair perfect visual acuity.
In other words the TARGET of the Main FUNCTIONAL COMPLEXES is a (stable pre-corneal) TEAR FILM . . . and the AIM is VISION.
Therefore it is no surprise, that the Japanese Dry Eye Society is focusing mainly on the Tear Film and states "In Japan, decreased tear film stability is regarded as the core mechanism of dry eye" and this society has developed a scheme for a "Tear Film Oriented Therapy" (TFOT) - this is available at http://www.dryeye.ne.jp/en/tfot/index.html.
The TFOT therapy approach appears to focus on the typical patient in clinical praxis. It does not so much focus on aspects of Surface Damage that is induced typically downstream of Surface Damage ... but may sometimes occur as a first primary pathology e.g. in malnutrition, in systemic disease or in alterations of regulatory systems.
Surface Damage can eventually lead to serious inflammatory pathways that may need anti-inflammatory therapy approaches of different kind than those directed to the tar film in order to prevent Degenerative Tissue Remodeling with Loss of Function of the Ocular Surface ...
Most patients with mild to moderate Dry Eye Disease in the more developed countries will have a primary problem with the tear film - therefore the TFOT approach of the Japanese Dry Eye Society appears as a practical and usable initiative.
Therapeutic MANAGEMENT of Tear FLUID in Dry Eye Disease
When we consider the above described physiology of tears at the Ocular Surface there are at least three different therapeutic approaches for the ´Management´ of Tear Deficiency in Dry Eye Disease. These interact with the three main phases of tears at the ocular surface which are:
SECRETION/ PRODUCTION inside the glands
RESIDENCE/ BATHING on the ocular surface (´bathing´ of the tissues) with potential evaporation
DRAINAGE/ DISPOSAL of the ´used´ tears by drainage via the lacrimal drainage system into the nose
The Management of Tears with respect to a Tear Deficiency at the Ocular Surface includes at least
... two sides of the same coin show that the MANAGEMENT OF TEARS and their deficiency, respectively, at the Ocular Surface can dissected into different steps which are: (1) The STIMULATION of natural tear flow by secretagogues, (2) the SUPPLEMENTATION of tear components either as individual components such as e.g. just lipids, or as a kind of complete solution as "Artificial Tears", and (3) the RETENTION time of the tear fluid at the Bulbar Surface before they disappear and drain into the lacrimal drainage system ... which also is a part of the Ocular Surface but can no longer keep the cornea and conjunctiva moist.
STIMULATION of Tear SECRETION
by Substances that are termed ´Secretagogues´ and act on the production rate of the ocular GLANDS
SUPPLEMENTATION of Tears
directly on the bulbar ocular surface. Unluckily impossible at present to imitate the complex arrangement of the tear fluid. Therefore typically ´Tear Components´ are supplemented, either aqueous or lipids or specific compounds. These are applied in the form of classic eye drops, or, by application as a spray, which can have some advantages at least for the elderly.
RETENTION of tears
on the bulbar ocular surface can be maintained by closing the outflow through the lacrimal puncta on the nasal aspect of the eye lids. This acts basically in the same way as closing the kitchen sink by a plug. There are permanant surgical ways to perform the closure of the puncta and non-permanent ways by so-called ´punctum plugs´ of different kinds. One principle concern is that the remaining low tear volume on the ocular surface of patients with dry eye disease may already be unsuitable and potentially detrimental for the surface tissue, either because the tears could be too hypertonic or because too many soluble pro-inflammatory mediators (please see there) have accumulated in the tears. These concerns may be overly academic because most patients with severe Dry Eye Disease who are using e.g. punctum plugs profit fro this therapeutic approach.
Tear Supplements should generally be FREE of PRESERVATIVES
A factor of utmost importance is, that tear supplements should NOT contain Preservatives because basically all of them act more or less destructive on the ocular surface tissues. After some decades of research , this is eventually sufficiently known and respected.
Nowadays, many supplements are luckily available in a preservative-free form that uses either disposable single-dose containers or multi-dose containers with refined techniques to keep the content of the container free of microbial infection.
LIPID SUPPLEMENTATION:
Therefore a primary lipid deficiency requires a primary supplementation with lipids !
HOW to Supplement ?
LIPID supplementation can be done in different ways - either in the form of eye drops that contain lipids and would have the advantage that they provide water at the same time ... or in the form of Lipid Spray where the lipid is stored in form of Liposomes.
The most sensible way - when only lipids are missing, which is the most frequent primary cause - would be to supplement only lipids. This would also be the ´cleanest´ approach in order to avoid introducing any unnecessary ingredients onto the ocular surface. In a practical clinical way ... certainly everything that works will be appreciated !
Another advantage of Liposomal Spray may be that it is easier to apply for elderly patients because there is no need to practice a single drop into the everted lover fornix ... but, instead, ... the liposomal spray can be applied onto the closed eye lids because the contained phospholipids finds their way, from the lid skin over the lid margin onto the ocular surface. This may also be of advantage for patients who do not like to touch their eyes too much - in this case, certainly contact lens wearers have a clear advantage because they have developed a reduced sensitivity and are more experienced to touch their eyes.
WHICH Lipids to Supplement ?
More tricky than the application form, which is often decided according to the patients preferences, is probably the questions, which lipids are missing from the plethora of different lipids in the Meibomian secretions. This question can presently not be answered by diagnostic tests but only by trial and error !
It is probably not so much the net amount of lipids on the ocular surface that is lacking but more important is the specific missing lipid species.
On the other hand the TearScience LipiView diagnostic instrument, that can measure the thickness of the tear film lipid layer (TFLL) with unsurpassed precision, typically shows low levels in patients with lipid deficiency. Still, not every patient with a lower than average TFLL also has Dry Eye Symptoms.
Symptoms may generally depend, as discussed for the nervous system in the section for ´Regulatory System´, on different levels of sensitivity in different individuals.
Of critical importance for the tear film lipid layer (TFLL) are amphiphilic lipids like phospholipids
Low TFLL values may also indicate, that not the pure mass of lipids but their specific function is decisive: Of particular importance in the relatively thin connecting layer of amphiphilic lipids, that are thought to be mainly phospholipids. They are probably joined by associated proteins.
Even tough the amount of phospholipids that can bind the superficial mass of non-polar lipids to the aqueous phase is small - they are very important. Missing amphiphilic lipids may explain why the hydrophobic lipids can no longer form a thick surface layer on top of them (please see the diagram above). This would explain low measurements for the TFLL, even though the lipids are principally there - but not in the right place and thus not in function.
AQUEOUS Deficiency & SUPPLEMENTATION
Dry Eye Disease is traditionally treated by mainly aqueous topical tear substitutes based on the observed lack of tear fluid and the symptoms of dryness and grittiness.
When a lipid deficiency is part of the disease process, as occurs in all cases of Meibomian Gland Dysfunction (MGD) - which is the main causative factor for Dry Eye - the sole use of aqueous tear supplements is usually of limited success.
With increasing destruction of tissues and regulatory systems in moderate to severe Dry Eye Disease the primary types of tear film deficiency tend to mix because the ocular surface becomes increasingly dysregulated. A main concept for aqueous tear deficiency is based on such dysregulation that occurs when the afferent sensory innervation at the ocular surface proper, cornea and conjunctiva is impaired and thus the neural reflex arc for tear secretion is altered resulting in lower aqueous secretion.
In moderate to severe Dry Eye Disease the types of tear film deficiency tend to mix
In moderate to severe Dry Eye the alteration of the ocular surface has typically involved more components of the tissues and of the regulatory systems The ocular surface functional unit thus becomes increasingly dys-regulated.
A major concept for explanation of aqueous deficiency is e.g. that, due to an impairment of afferent sensory nerve fibers at the wounded and/ or inflamed ocular surface, the driving force for the neural reflex arc for tear secretion becomes disturbed ... and therefore a lack of aqueous tears due to dysfunction of the aqueous system can occur in addition to a primary lack of lipids.
PATIENT SATISFACTION comes from efficacy of a tear supplement ... but also from the necessary frequency of application
THEN ... aqueous replacements certainly make sense IF a prevalent lipid deficiency is also treated - if not, the replaced aqueous solution will most likely have a limited half life on the ocular surface and evaporate soon ... with a need to repeat the dripping ... and so on. A satisfaction of the Dry Eye Patient comes to a large degree not only from the effectivity of a certain tear supplementation - which is certainly key - but also from the frequency with which the supplement has to be repeatedly applied during day-time.
HYALURONIC ACID (HA)
HA - The Gold Standard for Aqueous Supplementation
Different INGREDIENTS are used for aqueous solutions in order to hold the supplemented water on the ocular surface and to bind it to the surface for as long as possible in order to provide a certain degree of lubrication with is another important function of the tear fluid.
Hyaluronic Acid (blue) is a large bio-polymer with very high water-binding capacity. It typically occurs e.g. in the jelly-like vitreous body of the eye, in the viscous fluid of joints, and in connective tissue.
Hyaluronic Acid (HA) has become popular since about the millennium years HA is a large polymeric molecule with enormously high water binding capacity that is used in the body as a main component of connective tissue and in articulate liquid (synovial fluid).
The vitreous body, that fills the respective main cavity of the eye ball behind the lens, is almost completely composed of hyaluronic acid and the bound water. When we are young it is highly viscous like a thick jelly.
With advancing age the chain lengths breaks progressively down and the vitreous becomes increasingly liquid. Remnants of hyaluronic aggregates are then sometimes seen as ´flying moskitos´(mouches volantes) against bright sunlight.
Individual Hyaluronic Acid (HA) molecules with lots of bound water molecules are seen in the left image. On the right side the loose connective tissue of the Conjunctival Lamina propria is shown - where HA acts as a spacer between the collagen fibers (grey) and HA thus provides a certain elasticity to the tissue.
In connective tissue HA acts as a kind of spacer among the collagen fibrils and thus provides a part of the elasticity of our skin for example and also in the ocular tissues such as the conjunctival lamina propria. Its use in the articulate fluid indicates that it also has a lubricating function - that is certainly of advantage for a tear supplement in Dry Eye Disease.
HA used to be very expensive but has now become affordable
In previous decades HA used to be very expensive and was only used for intraocular surgery but nowadays due to advancements in synthesis, HA has become reasonably affordable to be used in aqueous tear supplements.
HA formulations can have different characteristics that allow some custom-tailoring according to the needs of the patient:
HA is available in solutions with different concentrations (i.e. amounts) of HA in water and in different molecular weight which refers to the chain length of the polymeric molecule.
The longer the chain length is the more viscous and gel-like the solution becomes, as discussed above for the vitreous body inside the eye. It might then negatively influence the visual acuity but it also stays longer on the ocular surface, which makes it particularly suitable for over-night use. High molecular weight HA is also difficult to filtrate as is sometimes required for sterile multi-dose dispenser systems.
The shorter the chain length of HA the more liquid and less viscous the solution becomes. The advantage is that is can be better filtrated in sterile multi-dose dispensers that depend on the principle of filtration for sterility. Another advantage is that the likeliness of causing visual disturbance is also lower with such solutions. A disadvantage on the other hand is, that the residence time on the bulbar surface becomes shorter and the solution must be re-applied more frequently.
Hyaluronic Acid Aqueous solution can assume lower viscosity during a blink - similar to the natural tears
Hyaluronic Acid has the principle advantage that it has some characteristics of a Non-Newtonian behaviour on the ocular surface which resembles the natural tears.
HA solutions have a higher viscosity, i.e. are more gel-like on the opened Obular Surface in the interpalpebral surface and thus stays more stable here.
During blinking however, HA-aqueous sultions show a certain distension of the ongish molecueles and thus achieve a somwwhat lower viscosity. i.e. is more fluid and thus reduces the friction during bliniking. This is ideal in order to support the natural nessesities of the Ocular Surface
This is in addition to the principle variation of characteristics of HA with molecular size and percentage of volume.
At present HA is probably the most wide-spread and probably the most useful additive to aqueous tear supplements. HA is the quasi Gold Standard for aqueous tear supplementation and new formulations with alternative ingredients and also tear secretagogues have to prove that they are superior to Hyaluronic Acid.
The enormous world-wide Variety of different types of tear supplements is difficult to oversee
The world-wide choice of different types of aqueous tear supplements, which are typically available over the counter and do not need to be prescribed is very large and almost impossible to oversee ... including all the different types of components ... not to talk about the different brand names. An overview of tear supplements thus exceeds the scope of this site. Other sites in the internet, however, sometimes deal exclusively with large overview of all possible tear supplements.
MUCIN Deficiency & SUPPLEMENTATION
Mucin Deficiency is relatively rare according to the presently available studies and publications - at least as a Primary Deficiency of Mucin as a major factor in Tear Film Deficiencies.
We know, however, a few FACTS about MUCINS at the Ocular Surface from the existing literature that may make us re-consider the above shown probably too simple statement:
already from the early systematic studies on Dry Eye Disease it was concluded that mucin is a critical component of the tear film because mucin was found as the per-requisite for adherence of the aqueous tears to the epithelial surface - termed wetting: No wetting - no tear film ... no tear film - Dry Eye Disease ... Hmmm
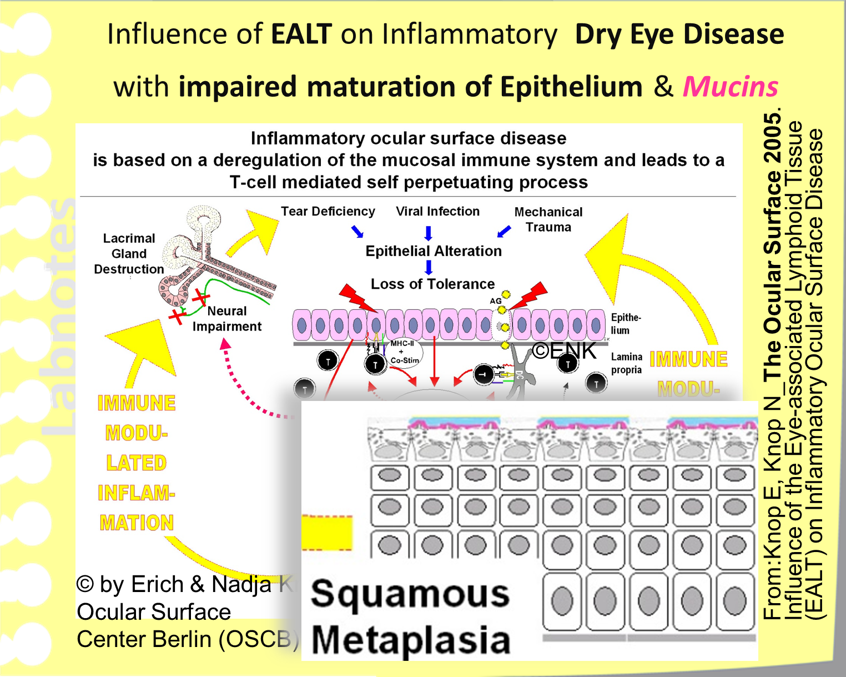
then we can conclude form the described patho-physiology of the disease process of wetting deficiencies that they tend to propagate via self enforcing vicious circles, that constitute a DYNAMIC PROCESS, into surface damage and thus into manifest Dry Eye Disease.
Manifest Dry Eye Disease with tissue pathology has an even higher tendency to propagate because it leads to onset of inflammatory amplification mechanisms.
... and in the chapter for surface damage it was explained that surface damage, even without inflammation, reinforces tear film deficiency, because it destroys the surface cells and thus the mucin layer - which leads to dry spots and wetting deficiency.
and then we know from studies of Steven PFLUGFELDER, Mike STERN and colleagues that the inflammatory process in dry eye disease and particularly inflammatory cytokines impairs the maturation of the epithelium with the result of immature surface cells without the normal integral glycocalyx mucins. Which again results in, or amplifies a, Tear Film Deficiency.
we have also heart, that, due to the DYNAMIC PROCESS of propagation and self-enforcement of the disease process, more and more Tissue Components are altered, wounded, impaired or destroyed and that the increasing deterioration of the tissue also the regulatory systems are affected and impaired
this meets very nicely with the observation by Mike LEMP and Tony BRON, that different individual types of tear film deficiency tend to MIX with increasing severity of Dry Eye Disease
SO ...by NOW ... it appears probably quite likely that a MUCIN DEFICIENCY will occur in more cases of Dry Eye Disease than it might be assumed from the frequency of a lack of mucins as a primary factor for Dry Eye Disease. This raises the question of ...
THERAPY OPTIONS for MUCIN DEFICIENCY
Unluckily there is not much in store in terms or mucins deficiency. In historic experiments mucins from non-human and from extra-ocular sources were used which does not appear as a suitable source for the therapy of Dry Eye Disease.
A potential supplementation of mucins as well as of aqueous secretion could be provided by SECRETAGOGUES - please see the next Chapter:
SECRETAGOGUES - Stimulators of Secretion
Secretagogues are natural substances or artificial drugs that stimulate the actual secretion of the secretory tissues typically by interacting with a specific receptor on secretory cells. The Targets in case of the Ocular Surface are:
the ocular gland organs
the single glandular cells (goblet cells) of the conjunctiva
... and also the ´ordinary´ conjunctival epithelial cells
since these also have the ability of secretion by:
secretion of membrane bound mucins
and of water
Thereby Secretagogues represent a different approach compared to the conventional artificial external supplementation or tear components by instead activating, re-activating or stimulating the own secretion of the patient.
P2Y2 receptors induce fluid transport at the ocular surface
Secretory cells of several Ocular Surface Tissues, as shown here in a schematic drawing, are equipped with cell membrane receptors for the agonist P2Y2 that allows a regulation of secretion
One interesting Secretagogue addresses the P2Y2 Receptors on epithelial cells.
P2Y2 Receptors are purinergic receptors - receptors that bind purins - adenosin or uridine nucleosides and nucleotides. These are nitrogen containing circular molecules such as ATP or UTP. Purin receptors are located in the cell membrane of many cells and therefore respond to extracellular signals from other cells or to mediators that are given as a therapeutic drug
P2Y2 Receptors are a subclass of purinergic receptors that are involved in the transport of ions, mainly chloride ions, and subsequently of water, through the cell membrane. P2Y2 Receptors occur in many cell types of the eye as reported by COWLEN and colleagues. At the ocular surface they occur in epithelial cells of the cornea and conjunctiva, including the goblet cells and also in Meibomian gland cells of the acini and the ducts. The water is transported through the cells by transcytosis - not along the para-cellular track between the cells because this is sealed by tight junctions.
P2Y2 receptors also promote mucin secretion and Meibomian gland function
Interestingly P2Y2 receptors do not seem to occur on the main and accessory lacrimal gland cells and are therefore not involved in the ´normal´ aqueous tear production.
P2Y2 receptors in the conjunctiva induce a unidirectional transport of chloride ions and water from the baso-lateral side of the connective tissue lamina propria, through the epithelial cells into the luminal tear fluid compartment as reported by LI and colleagues. P2Y2 receptors also promote the secretion of mucins from goblet cells and were reported to promote the function of the Meibomian Glands.
A NEW drug targets the P2Y2 receptor for stimulation of secretion in Dry Eye Disease
Secretagogues that stimulate the P2Y2 Receptor on ocular Secretory Tissues allow to target an increased secretion of tear components and thus an increase of tear fluid volume on the ocular surface. An example of this class of tear supplementation drugs is the P2Y2 agonist Diquafosol from Santen Pharma, which is however only available in Asia.
A drug became available in 2010 that targets the P2Y2 receptor for stimulation of secretion at the Ocular Surface. This secretagogue is presently only available in Japan and South Korea under the name of Diquafosol (Santen Pharma). Several studies have shown its safety and efficacy.
The effect of this secretagogue is very fast. According to a study by YOKOI and colleagues that, measured the pre-ocular tear volume over time by reflective meniscometry, in determining the change of tear meniscus curvature as a surrogate for tear volume, reported that the tear volume was significantly greater from 5 to 30 minutes after Diquafosol application in normal human eyes. The same group verified that also in Sjögren patients the drug significantly increased the tear meniscus after 15 minutes.
P2Y2 Laboratory and clinical studies have shown, that stimulation with a P2Y2 agonist indeed increases the release of secretory mucins from goblet cell source into the lacrimal fluid. Diquafosol significantly increased a marker for mucins in the tear film 5 minutes after application although the effect was transient and not observed at 15 minutes after application as reported by SHIGEATSU and colleagues. Data from impression cytology showed a decrease in the diameter and amount of mucin impressions from goblet cells after the application of Diquafosol which points to the release of secretory mucins which is in line with the data on mucin content in the tear film as measured in the previous study.
Another study by ARITA and colleagues reported that topical 3% Diquafosol with application 4 times a day one drop over a time of 4 months in Dry Eye Patients with Meibomian Gland Dysfunction (MGD) improved the signs and symptoms of Dry Eye Disease. It was also reported to increase the relative amount of the Gland tissue as detectable in non-contact Meibography slightly by 4,6%. Since P2Y2 receptors also occur on Meibomian gland epithelial cells the results may indicate that this secretagogue can also act positively on the Meibomian glands.