Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT ]
DEEPER
INSIGHT
The ´SCIENTIST´s Page´ is open to those with deeper interest
... in the OCULAR SURFACE and DRY EYE Disease
Choose a CHAPTER of your interest - or just follow the illustration ... which is perhaps the most informative
THE EYE SURFACE
The surface of the eyes must be constantly moist to remain healthy and to achieve perfect visual acuity
What IS the eye surface?
=> The moist mucous membrane tissue on the front of the eye!
The OCULAR SURFACE is the moist mucous membrane tissue on the front of the eyeball.
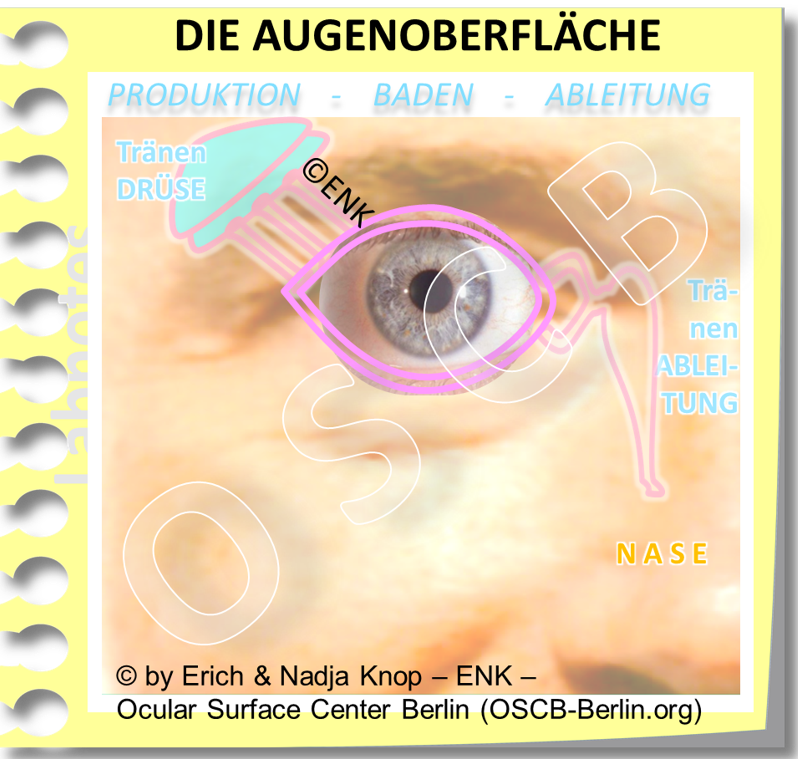
In addition to the visible cornea and conjunctiva, which are bathed in tears, the surface of the eye consists of organs hidden under the skin: from the attached lacrimal gland for the production of new tears to the lacrimal drainage channels for the removal of the ' used ' tears into the nose. The tears enter the drainage system through the lacrimal puncta at the nasal side of upper and lower eyelids.
In this drawing, the depth of is conjunctival and the thickness of the tear film is exaggerated, so you can see them - in fact, the eyelids are literally right on the eyeball, the conjunctival sac forms only a wet gap, and the tear film is extremely thin.
The CONJUNCTIVA is a support tissue of the cornea, which contributes significantly to the health of the cornea and the whole eye.
It covers the front of the eyeball and the back of the eyelids by forming the conjunctival sac. The conjunctiva therefore connects the surfaces of the eyeball and the eyelids.
The conjunctival sac is only open to the outside world in the area of the open eyelids, i.e. the interpalpebral fissure. There, the tissue must be covered with a thin film of tears - the tear film that keeps the sensitive cell surfaces always moist, even when the eye is open.
Why does the surface of the eye have to be moist ?
=> To maintain their health and integrity for the transparency of the cornea !
Only a MOIST cornea is TRANSPARENT
The MOISTURE surface of the eye is needed to the cornea / cornea TRANSPARENT keep
The surface of the eye is a moist mucous membrane to keep the cornea / cornea transparent.
The surface of the eyes must be kept permanently moist - always and everywhere - in order to remain intact and healthy and is therefore constantly bathed in the tear fluid.
TEARS are the medium for the moisture at the ocular surface
The continuous flow of tears over the surface of the eye , which is of the utmost importance for your health, goes (from left to right in the illustration): (1) from the main production site in the lacrimal gland via (2) the visible cornea / cornea and conjunctiva / conjunctiva that must be constantly bathed in (3) the lacrimal drainage system , the ' used to derive' tears into the nose.
The tear fluid is formed by the glands at the surface of the eye and after ´use ´ - that is, after bathing the cornea and conjunctiva - the ´used´ tears are transported into the nose by the draining tear ducts.
The continuous new production of tears and the tear flow along the ocular surface is therefore of the greatest importance for your health and for the clarity of the cornea - i.e. for intact Vision.
It is important to remove the 'used' tears in a controlled manner, as there is only space on the surface of the eye for a very small tear volume.
... in fact it is the case that not even a single additional drop of liquid, e.g. from eye drops, has space on the surface of the eye. After applying an eye drop, often most of the liquid runs off again via the edge of the lid.
In contrast to a really 'dry' eye, a temporary increased tear production due to eye irritation can result in episodes of a 'watery wet dry eye'.
Also a disturbed removal of the 'used' tears from the ocular surface, due to obstructed lacrimal puncta, can lead to tears overflowing over the edge of the eyelid.
... we can therefore see that the conditions on the surface of the eye do not differ significantly from our experience in other areas of daily life - both 'too much' and 'too little' can be annoying ;-)
What is the tear film- and what is its function?
=> A multilayered liquid sheat on the eye that ensures moisture and clear vision when the eyelids are open !
Constant moisture for the cornea and conjunctiva in the area of the open eyelid cleft is made possible by a thin layer of tears - the tear film.
It is thin and even enough not to disturb the visual acuity and at the same time sufficiently stable to prevent the tissue from drying out due to evaporation of the tear water in the air atmosphere.
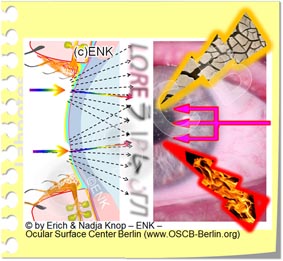
The uniformity of the tear film is of great importance for the perfect visual acuity because the tear film is the first refractive surface of the eye.
Faults and irregularities in the tear film with a lack of tears in dry eye but also with excessive tearing in a wet ´dry eye´ are often first manifested by reduced or fluctuating blurred vision (unstable visual acuity).
The TEAR FILM (left) consists of 3 layers, the components of which are produced by 3 different types of eye glands (right).
The tear film has three layers , which consist of the products of the different glands of the eye surface :
Mucus (mucin ) from individual goblet cells in the conjunctiva forms a thin layer on the cells and only makes the tissue surface wettable for water.
Water , which is the main body of tears, is produced by the lacrimal gland, which is located on the side of the eye socket.
Oil is produced by the meibomian glands in the eyelid and forms a very thin layer on the surface of the tear film - similar to oil on a puddle of water on the roadside. The oil reduces the evaporation of the water and improves the stability of the tear film.
A look into the tear film
A LOOK INTO THE TEAR FILM: The middle main part of the tear film in front of the transparent cornea consists of aqueous liquid. The numerous finger-like extensions (micovilli) of the superficial epithelial cells are visible below - they bind the water to the cell surface. The water is bound by the long sugar chains (here reddish) of mucins. Membrane-bound mucins (glykokalyx) are fixed to the microvilli whereas soluble mucins float in the tear film and transform the water into a low-viscosity water-mucin gel. At the top, the tear film is covered by the very thin layer of oil from the fats of the meibomian glands - this prevents the tear water from evaporating too quickly.
What role does the cell surface of the eye play?
=> Only the intact fine structure of the surface of the eye enables moistening with the watery tears
The intact cell surface is an indispensable prerequisite for moisturizing the eye and thus for eye health.
The cell surface produces mucins that allow the surface to be wetted:
unicellular goblet glands produce soluble mucins. Together with the water from the lacrimal gland, they form a mucin-water gel - this is the main part of the tear film.
all cells form membrane-bound mucins, which are firmly anchored in the cell membrane and bind the watery tears to the cell surface.
In addition, some soluble mucins also come from the lacrimal gland
The cells have numerous fine finger-like extensions that increase their surface area and thus improve water binding.
... accordingly, damage to the cell surface (mechanical or chemical) with destruction of the fine structure leads to disturbances in wetting with tear fluid and to increased dryness and irritation of the eye.
Electron microscopy shows the tiny structures on the surface of the eye
Goblet cells
Goblet cell glands in the conjunctiva produce soluble mucins and release them to the surface in the tear film. They are already visible in the light microscope.
Goblet cells and mucins are marked in pink in the image.
Mikrovilli
The entire cell surface is covered with numerous finger-like protuberances (microvilli and microplicae / microfolds).
these are so small that they can only be clearly recognized by electron microscopy (please see image
Glycocalyx
In the cell membrane of the micro-processes are membrane-bound mucins. They appear as fine tree-like structures (glycocalyx, please see image) and protrude into the aqueous tear film to bind the water.
According to studies, this molecular arrangement is the basis for wettability of the ocular cell surface.
What role do the eyelids play?
=> The eyelids distribute the tears to the important tear FILM in the open eyelid on the surface of the eye!
This schematic simplified animation of the blink movement of the eyelids illustrates the basic function of the eyelids to distribute the tears into a thin film in the area of the eyelid cleft. This allows to keep the tissue of the ocular surface moist even when the lids are open to see. However, actual tear drops (as simplified here) occur in the area of the eyelid cleft only with excessive tear flow.
The eyelids are very important for the health of the eye.
The wiping movement of the upper eyelid when LIDSCHLAG
spread the tears in the thin and even tear film.
it will also squeezed oil from the meibomian glands in the eyelids
and spread the oil on top of the tear film.
The tear film is used to keep the tissue in the open eyelids open and is also the most important surface for correct refraction of the incoming light for perfect visual acuity.
Necessary conditions for a stable tear-film and thus for a healthy eye surface and a perfect visual acuity are sufficient in quantity and quality production of tear fluid by the glands and the formation of a sufficiently stable tear-film through the intact function of the eye lids.
... accordingly damage or negative influence on gland function and / or on the eyelid function can lead to a "dry" eye condition, i.e. an irritation with all the downstream consequences. if this condition becomes chronic, it can pass into the disease of the "dry eye".
WHY is the surface of the eye so important?
=> The healthy surface of the eyes is a prerequisite for VISION !
The healthy ocular surface allows a clear window for the eye to see the light from the environment.
Without a healthy eye surface, all later steps in the visual process become meaningless.
Deeper INSIGHT into ...The DRY EYE
The DRY EYE is a disorder of the permanent moistening of the surface of the eye with a disorder of visual acuity and subsequent damage to the tissue. This then leads to the patient's complaints and to the clinical findings of the surface damage
What is the DRY EYE?
=> The dry eye is a DEFICIENCY of the constant moistening by the tear film - mostly with subsequent tissue damage
The 'DRY EYE' disease is also medically referred to as " keratoconjunctivitis sicca " (KCS), ie " dryness inflammation of the cornea and conjunctiva " or, shorter, as sicca syndrome (dryness syndrome).
Interestingly, the formation of the oil layer in the tear film is of greater importance than the formation of tear water, because if there is a lack of oil, even abundant tear water evaporates quickly. Gaps are then created in the tear film and the sensitive cells on the surface of the eye are damaged.
Colloquially, the terms 'dry eye' , ' burning eyes ', ' heavy eyelids' or 'tired eyes ' ... as well as many other terms are common, which in one way or another suggest that the surface of the eye is irritated.
The DRY EYE is a complex regulatory disorder of the functional anatomy of the surface of the eye, which reduces the permanent moisture of the tissue and thus its health and perfect visual acuity .
This is typically accompanied by subjective symptoms of various degrees of irritation and pain on the surface of the eye as well as clinical findings of tears and corresponding tissue destruction as well as disorders of visual acuity , mostly in the sense of fluctuating visual acuity or blurred vision.
Rarely, tissue damage can also occur first in a sicca
This happens when the disorder of the tissue surface is caused by another underlying disease. Then a dry eye can appear due to primary tissue damage, which only leads to tear film disorders afterwards. Examples are:
a nutritionally strong vitamin A deficiency or
a local or systemic inflammatory disease
the chronic effect of cell-damaging preservatives in eye drops, especially if they are dripped over a long period of time and several times a day
In more developed countries, systemic inflammatory diseases are more common than primary tissue damage in a sicca. With the increase in bone marrow transplants, the number of rejection reactions in the sense of a ‘ graft-versus-host disease’ (GvdH) , which can also affect the eye and then often trigger a sicca.
In less developed regions of the world, on the other hand, primary tissue damage due to a nutritionally strong vitamin A deficiency is unfortunately still common. The squamous metaplasia of the conjunctiva (see figure) in the emerging sicca is then even used as a diagnostic marker for the vitamin A deficiency.
Symptoms of Dry Eye Disease
What are the typical symptoms of a DRY EYE?
Typical subjective SYMPTOMS are different degrees of eye dryness, blurred vision, eye irritation and pain!
The basic causal factors of insufficient tear production and / or insufficient spread of a (sufficiently stable) tear film ...
... lead to the basic pathologies of the dry eye, namely the instability of the tear film and the subsequent drying and damage to the tissue.
These two pathologies explain the typical symptoms of the dry eye:
feeling of dryness
the feeling of dryness is perhaps the most common and therefore eponymous complaint - although many other symptoms are possible
wet eye
initially there may occasionally be an increased flow of tears and ´ watery eyes´ alternating with dry eyes
... this is triggered by a reflex activation of the tear production - a protective reflex of the surface of the eye
irritation and pain - to varying degrees
sandy gritty feeling, foreign body sensation , burning and stinging
dull feeling of pressure around the eye and even behind the eye is possible
this also explains the common description of the dry eye as:
'heavy' eyelids or ' tired' eyes
' Heavy eyelids' and 'tired eyes ' describe the subjective perception of constant increased friction between the eyelids and eyeball during chronic dryness and tissue irritation
fluctuating visual acuity / blurred vision
Visual disturbances are common and usually consist of occasional blurred vision or fluctuating visual acuity - they result from an uneven thickness of the tear film and are typically improved by blinking several times.
increasing problems with contact lens wear
Since contact lenses place increased demands on the tear film and also the evaporation of the aqueous tears increases, there is an increasing incompatibility of contact lenses , especially soft hydrogel contact lenses
redness
an eye redness is typical in chronic irritation - but usually not very pronounced in mild to moderate dry eye
It is typical of the dry eye that the subjective symptoms do not always exactly match the clinical findings .
Clinical findings
What are the typical clinical findings of dry eye disease ?
Typical dry eye clinical findings are
decreased tears ,
low stability of the tear film , and thus insufficient wetting of the tissue
Damage to the tissue surface leads!
The animated schematic drawing shows a very unstable tear film. Here, after a blink of an eye, it only remains stable for about a second before it opens. This indicates a strong disruption to the system and suggests subsequent tissue damage .
the stability of the tear film is determined by the Tear Film Break-Up Time (BUT)
is typically examined by staining the otherwise largely invisible tear film with a blue-green vital dye (fluorescein)
the normal value should be at least 10 seconds are to the tear film break up and thereby initiating a new blink , which then propagates a new intact tear film.
At the onset of dry eye disease, there may also be occasional episodes of increased lacrimation with watery eyes , which alternate with dry eyes
=> Further information can be found HERE
Defects in the cell surface / vital staining (normal: no staining)
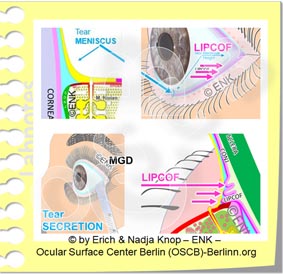
A moderate dry eye typically shows only a slight reddening of the conjunctiva and possibly the edges of the eyelids. The openings of the Meibomian sebaceous glands are often blocked by visible or invisible thickened secretion - this is the most common main cause of the dry eye. Surface defects appear in vital staining with fluorescein as superficial punctate keratitis (KSP).
An unstable tear film triggers dry spots in the epithelium of the surface of the eye due to the frequent, early opening.
There, the surface epithelium is disturbed by two major damage mechanisms ( secondary pathogenetic factors ): increased mechanical friction and increased osmolarity.
The injured, dried cells can be stained on the cornea with the vital dye fluorescein . On the conjunctiva, lissamin green usually stains better. The defects appear as small spots of staining (as keratitis superficialis punctata , KSP) in biomicroscopy with a slit lamp. You can find more detailed information on vital staining => HERE .
=> This vital staining is another important test for the dry eye, since it shows the severity of the dryness of the tissue damage and thus the dry eye.
Aqueous Tear Production Disorder ( Normal:> 10mm )
With moderate to advanced dry eye, the aqueous tear production is often disturbed - either in the sense of a reduced aqueous production or, occasionally, as excessive secretion.
Mostly (in 4 out of 5 cases) in dry eye oil deficiency in meibomian gland dysfunction with subsequent hyperevaporation is the primary cause of dry eye. But damage to the tissue, including the nerve fibers, can lead to disturbances in neural autoregulation of tear secretion.
It is therefore useful to have an orientation impression of the production performance of the lacrimal gland for the watery tears.
The appropriate test for the maximum production capacity of the lacrimal gland is the Schirmer 1 test (without prior local anesthesia). It is therefore advisable to carry out a preliminary determination of the tear film stability and a subsequent vital staining with fluorescein without the addition of a local anesthetic.
REDUCED TEAR VOLUME
on the surface of the eye
(mostly) by increased evaporation of the tear water - as ' evaporative dry eye' called ... or
(much less often) due to a reduced amount of (aqueous) tear secretion from the tear gland
referred to as ´ primary watery tears ´
diagnostic
wird ein effektiver Tränenmangel an der Augenoberfläche am einfachsten festgestellt durch eine Beobachtung oder Vermessung des Tränenmeniskus.
weiterführend sind: Tränenfilm-Tests und Drüsen Tests
ÖL MANGEL
(nach Menge oder Qualität oder beidem) mit Störung der Lipidschicht auf dem Tränenfilm und nachfolgender verstärkter Verdunstung
dies ist eine typische Folge der Meibomdrüsen- Dysfunktion´, (MDD) - sieist der Hauptgrund für ein Trockenes Auge.
Diagnostisch:
lässt sich die Funktion der Meibomdrüsen am einfachsten prüfen durch eine ´Diagnostische Expression´
Genauere Diagnosen und Quantifizierungen werden möglich durch Interferometrie und Meibographie.
Verschwinden von Meibomdrüsen Gewebe
(im Engl. bezeichnet als ´Gland Drop-Out´) bei der optischen Betrachtung (Meibographie) der sonst nicht sichtbaren Meibomdrüsen, die versteckt im Augenlid liegen.
Veränderungen am Lidrand wie:
Schaum und Ablagerungen auf dem Lidrand durch veränderte Fette der Meibomdrüsen
verstärkte Rötung und verstärkte Füllung der Blutgefässe
Demodex Milben an den Wimpern
blocked meibomian gland openings with protrusion or leaked hardened fats of the meibomian glands
Rounding and irregularities of the back edge of the eyelid
Epithelial damage => KSP
Increased friction and increased tear film osmolarity in tear film disorders lead to damage with defects in the surface of the eye. You can find more detailed information on vital staining => HERE .
This affects the surface epithelium first and can be demonstrated by staining with vital dyes . Defects occur:
on the cornea / cornea and conjunctiva / conjunctiva as superficial punctate keratitis (KSP)
but also on the back edge of the lid edge - as a lid wiper epitheliopathy (LWE)
Increased amounts of inflammatory mediators
Inflammation mediators are typically formed by dry eye tissue destruction and occur in tears and tissues. These are various factors, e.g.
inflammatory cytokine and chemokine signaling substances
subsequent activation of tissue-degrading enzymes (matrix metalloproteinases, MMP ).
The most common protease (MMP9) on the surface of the eye can be diagnosed with a rapid test .
Damage to the connective tissue => LIPCOF
If the surface damage progresses and inflammatory reactions occur, the connective tissue underneath the epithelium is also damaged. Here typically occur Li dkanten- P arallele Co njunctivale F old ( LIPCOF on).
LIPCOF are the sign of advanced tissue destruction through the activation of tissue-destroying enzymes , mostly matrix metalloproteinase (especially MMP9).
Due to the tissue destruction, the conjunctiva becomes increasingly looser and ´folds wrinkles´. They already occur due to the low forces of the normal blinking of the eye over the surface of the eyeball. The rear edge of the eyelid then pushes the loosened conjunctiva in front of you like a snow plow when gliding over the globe.
Diagnostically are LIPCOF wrinkles in the slit lamp easily evaluated - better after staining of the tear film with fluorescein.
Nervous system regulation
The surface of the eye is regulated by the nervous system from the peripheral nerves and the central nervous system.
Important functions such as tear secretion and sufficient blinking are automatically regulated by reflex. At least when blinking, there is an arbitrary influence. For example, arbitrarily performed blinking and particularly powerful blinking are possible, which can help to improve the moisturization of the eye.
Stimulus and neural regulation of lacrimation and blinking
The sensory irritation of the surface of the eye in the dry eye, for example through drying, rubbing, hyperosmolarity or injury, reaches the central nervous system (CNS) via the eye nerves (cranial nerve V, trigeminal nerve).
The signals are processed there and the function of the eye is automatically regulated in the brain stem as required.
For example, the flow of tears and blinking are regulated via nerves that run back from the brain stem and brain to the eye (cranial nerve VII, facial nerve).
This also explains why chronic irritation in dry eye occasionally on overshooting irritant secretion and 'Wet eye' can lead
Excessive tear formation is a protective reflex of the eye , in which, in itself, a useful experiment simply ´wash away´ a ´excitement´, like a foreign body on the surface. With chronic irritation in the tissue itself, however, this cannot work.
At the same time, signals also reach the cerebral cortex, so that this can be perceived consciously and can also be reacted to when necessary.
Eyelid regulation - normal, rare or incomplete blinks
The processing of the signals from the surface of the eye is complex and is influenced by various centers in the CNS.
In principle, the blinking is controlled by the blinking reflex. When the tear film on the surface of the eye breaks open, the tissue begins to dry out, irritating the nerve endings there.
This triggers a blink of an eye, which spreads a new, even tear film and thus makes the nerve stimulus disappear again.
The reflex blink of the eye happens largely unconsciously, although a blink of the eye can of course be perceived consciously and also controlled consciously.
Rare eyelid blinks
With increased attention due to strenuous visual tasks, eyelid blinks can be deliberately delayed or suppressed
This affects many everyday activities, e.g. reading , especially on computer screens , watching TV or driving a car , especially at night, etc.
Then the eye is kept open longer so as not to interrupt the 'important' visual impression, even if a dryness stimulus comes from the surface of the eye.
In the illustration, the eye turns red due to the irritation before the blink of an eye finally occurs.
The eyelid blinks can then occur significantly less than the normal value of approx. 5-10 times per minute. Since the tear film is only stable for about 10-20 seconds , the surface of the eye can dry out easily.
So rare blinking can create or worsen dry eyes.
On the other hand, not only the frequency but also the complete sequence of blinking can be influenced.
With ´nervous blinking´ due to lack of concentration, nervousness, or habitually, eyelid blinks can be done more often than necessary and are often incomplete without being consciously noticed.
Incomplete blinking means that the upper eyelid does not close completely when the eyelid is closed (please see animated image). Therefore, the tear film cannot be completely renewed. The lower part of the tear film then always remains relatively dry and there is increased damage to the cell surface .
Incomplete blinking is quite common and is therefore a common co-factor in dry eyes. However, they are not noticed by the patient and are sometimes difficult for the doctor to diagnose without special equipment .
Irritation and processing to feel pain
The neuronal regulation of the surface of the eye, via the cranial nerves V ( trigeminal nerve ) and VII ( facial nerve ) in the brain stem, and also their emotional perception in the brain is complex. It is susceptible to interference, but it can also show certain individual differences between different people. Experiences, evaluations and different types of treatment and processing of events on the surface of the eye are also included here. It is also an experience of everyday life that the ' nerve costume ' can be a little different for every person.
In principle there is a certain difference between the pure ´perception´ of a stimulus from the surface of the eye that occurs in the cortex and the evaluation of these stimuli in the ´subordinate´ Limbic system.
´Pain´ is not a perception in the actual sense, but a construction of the brain .
This construction results from the emotional evaluation of a perception. The evaluation takes place above all in the so-called limbic system and through other emotional instances. Numerous other things, such as experiences and expectations, etc., flow into the subjective evaluation.
However, for the individual person the two instances of ´perception´ and what appears as ´pain´ are not always to be clearly separated. So in the end it is not always clear which of the various instances in the brain is ' cook or waiter ' .
On the surface of the eye, this means that the strength of a stimulus on the surface of the eye and the feelings of pain that the patient perceives subjectively are not always closely related.
Difference between clinical findings and patient perception
Why do the SYMPTOMS of the dry eye often not match the clinical FINDINGS?
=> ... this has not yet been fully clarified and is the subject of current research!
It is typical of the dry eye that the severity of the patient's subjective symptoms in terms of pain does not always match the clinically detectable findings .
Subjective evaluation
Therefore, the subjective evaluation of a stimulus from the surface of the eye can dominate over the objective perception. This can depend on the ´day form´ of the individual person, but it can also be very different for different people.
This can be expressed in such a way that the subjective symptoms cause the patient to suffer a great deal of suffering while little or sometimes no objective findings are clinically detectable - this may be a pain syndrome .
On the other hand, however, a patient with significantly pronounced clinical findings, for example a surface damage that can be stained, may have little or no subjective symptoms in the sense of irritation or pain. Such a patient will then probably have little inclination to medically indicated therapy.
Pain syndrome
Disorder of pain processing can lead to pain syndrome.
Pain has the biological meaning to indicate damage to the body and thus give a signal for danger. With chronic chronic pain stimuli , disorders in the area of the pain system can occur. Routes of transmission of the nerves in the pain system can then be cleared and increasingly solidified. Then pain may persist, even if the pain stimuli on the body decrease or the tissue damage has already healed.
It has lost its actual meaning as a warning signal and becomes part of the disease. These pains are described as “neuropathic” pains
This means that a subjective impression of pain can continue to exist for the patient, even though successful treatment of the dry eye has already improved the condition of the surface of the eye.
Psychosomatic influences
Psychosomatic influences on a disease process and on the patient's perception have been an established and serious part of medicine for many years. In addition to, for example, non-specific back pain, functional cardiovascular problems or indigestion, this can also play a role in the dry eye , according to many studies .
If dealing with the disease becomes the most important part of life, this could be an occasion to seek psychosomatic help .
HOW does a dry eye develop?
... and how does it become CHRONIC? ? ?
Dry eye is strongly influenced by regulatory systems and risk factors
Various factors influence the function of the surface of the eye
A disruption of positive factors and the appearance of negative factors (risk factors) worsen the normal functioning of the tissue and therefore increase the risk of the appearance of a dry eye and the severity of the disease.
The complex disturbance of the function and structure of the surface of the eye in the dry eye leads to a lack of the basic functional complexes for the constant moisturization of the tissue.
The development of a dry eye is favored by several factors:
REGULATORY SYSTEMS
Disruption of regulation
Disorders of the nervous system, the endocrine hormone system and the immune system impairment the function of the surface of the eye.
Age and female gender (in connection with a relative lack of 'male' androgen hormone and an excess of 'female' estrogen) have a significant influence on the surface of the eye.
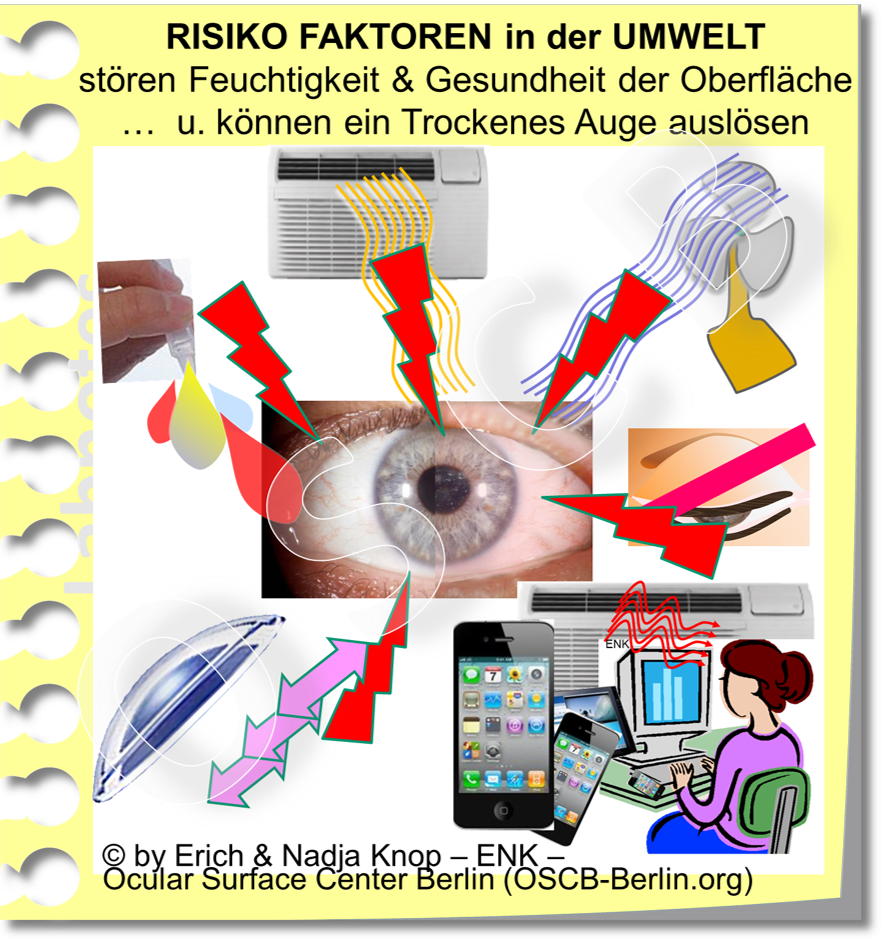
EXTERNAL RISK FACTORS
mostly have a drying effect
Negative external influencing factors are RISK FACTORS for the disease. They affect the TEAR FLUID on the eye and over claim the normal function capacity - but are often easily influenced. It is mostly drying environmental influences such as heat, drought, wind - even concentrated visual tasks with rare blinking of the eye. In climatic-ized office environments with VDU these risk factors are often combined and may be so for dry " office eye " (Engl. " Office Eye cause").
INTERNAL RISK FACTORS
Disorder of the organs
Negative internal influencing factors are also RISK FACTORS for the disease.
They affect the TISSUE that produces the tears and can worsen the normal function of the surface of the eye.
These are, for example, age and gender, as well as chronic illnesses or chronic medication, nutrition and drinking volume etc.. Many of these internal risk factors are difficult to influence.
Why does the dry eye tend to get worse?
... without adequate therapy
=> Tear deficiency with reduced moistening of the eye surface and subsequent tissue damage have a negative impact and reinforce each other!
Self-reinforcing inflammatory mechanisms
The complex pathological changes in the dry eye influence each other and form self-reinforcing control loops, which are often referred to as vicious circles.
This often leads to exacerbation of the disease if insufficient therapy is given.
Inflammation is an important enhancement mechanism
Inflammation is a powerful mechanism for the exacerbation of dry eye disease.
Inflammation is a basic mechanism for cells to defend themselves. against wounding and damage. This also typically occurs in dry eyes due to the instability of the tear film and the subsequent increased mechanical friction and increased osmolarity of the tear film.
Inflammation mechanisms cause tissue destruction to overcome the supposed pest and should then lead to tissue repair.
In diseases like the dry eye, ongoing tissue damage can lead to chronic inflammation.
If the inflammation becomes chronic, then it turns into a negative and destructive process because the initial tissue destruction cannot be replaced by an adequate repair and thus becomes increasingly severe. This creates self-reinforcing control loops (' vicious loops ') of worsening of the disease.
This powerful mechanism can significantly worsen the disease process.
In such cases of moderate to severe dry eye, it often makes sense if the treatment contains temporarily anti-inflammatory therapy approaches in addition to tear substitutes and physical lid margin therapy with lid margin hygiene .
For detailed information about dry eye therapy, we refer to the longer English language version of the OSCB information portal.
When does a "dry" eye become dry eye disease?
If a ´dry´ eye becomes chronic - then an occasional, temporary disorder can develop into a chronic DISEASE!
An occasional “dry” eye is not a disease
Most of us have probably already had a temporary feeling of 'dry' eyes, for example when we were exposed to unusually strong drying environmental influences. These are, for example, low air humidity, high temperature, wind, or rare blinking when working concentrated in air-conditioned room air.
Such a ´dry´ eye is typically a short-lived condition, which quickly improves and disappears when we become aware of it and increasingly blink or leave the drying environment.
When “dryness” becomes chronic ... this condition can turn into a disease
Only if the feeling of 'dryness' persists and cannot be improved by avoiding drying out environmental factors and by increasing, consciously and intensely blinking ...
… Then the temporary condition becomes chronic and an occasional “dry” eye can progress to the disease of the dry eye.
This is typically associated with an increase in the DURATION and SERIOUSity of symptoms and clinical findings due to increasing disruption and damage to the surface of the eye. Some important risk factors favor the appearance and severity of the dry eye.
Many different and mutually influencing self-reinforcing control loops of the exacerbation of the disease (often referred to as ´Develskreise´, English ´VICIOUS CIRCLES´) occur in the chronic dry eye and can lead to the clinical full picture of a chronically progressive tissue destruction with a loss of function of the eye surface to lead