Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT ]
OVERVIEW
The ´doctor´s page´ will deal with:
PHYSIOLOGY surface of the eye
PATHOPHYSIOLOGY in the dry eye
Typical SYMPTOMS
Important FINDINGS
Pioneering DIAGNOSTIC TESTS
SEVERITY division
THERAPY Step Plan
Please choose a TOPIC of your interest by clicking on an image - or just follow the presentation on this page ... which is perhaps the most informative
Basic PHYSIOLOGY
of the ocular surface
The surface of the eye is a permanently moist tissue
The OCULAR SURFACE is the permanently moist mucosal tissue on the front of the eyeball.
The tear glands and the draining tear ducts form the mucosal adnexa and belong to the surface of the eye.
The indispensable moisturizing, and thus eye health, is maintained by a few basic functional complexes.
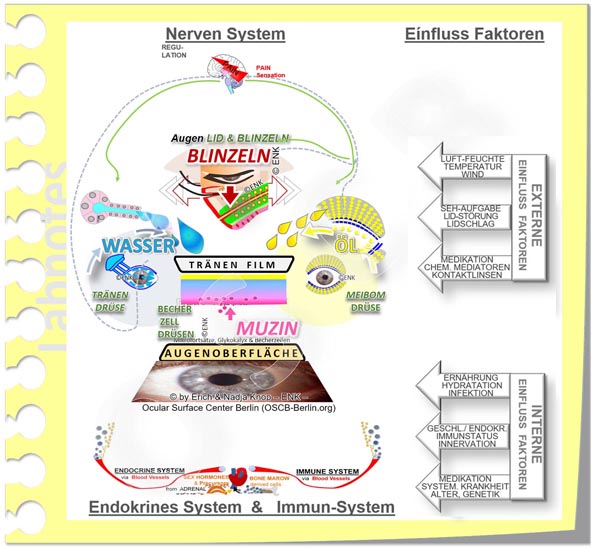
Basic FUNCTIONAL COMPLEXES
2 essential functional complexes ensure the moisture of the ocular surface as a basic requirement for its health:
Tear production
Tear distribution into the tear film
The eyelids spread the tears within the interpalpebral cleft into the extremely important thin tear film
Only the tear film can secure the moisture on the eye even when the lids are open - and at the same time it improves the refraction of light for optimal visual acuity.
A new vision of the ocular surface
The observation of the ocular surface via its functional complexes, which are important for intact function and thus also for the maintenance of structural integrity, results in a new image of the ocular surface.
The schematic representation of the functional complexes in their interaction as pictograms is intuitively understandable.
This new image leads to a holistic and dynamic concept of the ocular surface and from there to a holistic dynamic concept of dry eye disease.
The intact cell surface with its goblet cell glands is important for the wettability of the ocular surface:
The goblet cell glands (pink in the image) in the conjunctiva produce soluble water-binding mucins to form a mucin-water gel in the tear film
the intact cell surface is an indispensable prerequisite for eye health.
numerous micro-processes (microvilli and microplicae) and the integral mucins of the glycocalyx in their cell membrane allow the aqueous tears to adhere
= these structures can only be seen in the electron microscope .
PATHOPHYSIOLOGY of dry eye disease
Various factors are involved in the pathophysiology of dry eye disease and are explained individually below. Finally there is a summary.
Triggering CAUSAL FACTORS
Triggering causal factors for dry eye are disorders that lead to the formation of an insufficient tear film. Above all, these are:
Deficiency of tear production
quantitative or qualitative
by the various glands of the eye
the dysfunction of the meibomian glands is the main cause of a dry eye, according to current knowledge.
including the intact cell surface with goblet cell glands and mucin formation.
Deficiency of tear film distribution/ spreading
due to any disorder of the eyelids themselves or of their regular blinking movement, e.g. by:
Neural regulation disorders
Shape and position of the eyelids
is typically disturbed in the normal aging processes, when the eyelid tension decreases or the eyelid shape is twisted by a scarning condition.
Primary PATHOLOGY
The two primary pathologies in dry eye are
Tears film deficiency and
Tissue damage
Both pathologies are called "primary" because both of them can occur first and then induce the other one.
A typical consequence of the tear film disorder is damage to the sensitive cell surface .
this is clinically detectable as vital staining surface speckle (keratitis superficialis punctata, KSP), usually by using fluorescein.
Later there can be extensive damage with a degenerative remodeling of the tissue
Rarely, the tissue of the surface of the eye is damaged first, which can later lead to disorders of tear adhesion and thus moistening.
Secondary Pathogenetic Factors … occur as consequences of tear film deficiency and tissue damage
Subsequent secondary pathogenetic factors develop in both primary pathologies of the dry eye (tear film deficiency and tissue damage):
they are interlinked and
drive the disease process forward in cascades
the secondary factors can be collected as clinical findings
a severity stage of the dry eye can be classified based on these findings
TEAR FILM deficiency
With tear film deficiency, it is not always easy to assign the secondary pathogenetic factors exactly to the deficit of a certain tear component, ie a lack of
or to blinking disorders
According to the current understanding, in addition to a generally possible decrease of the visual acuity, the following assignment of symptoms can be carried out:
Aqueous tear deficiency ... leads to
Wetting problems with the development of 'dry spots' in the tear film
Increased mechanical friction .
due to reduced lubrication between eyelids and globe
is exacerbated by wearing contact lenses, especially if there is a lack of aqueous tears.
Chronic mechanical irritation
leads to tissue remodeling and is an inflammatory stimulus
Lipid / oil deficiency ... leads to
Tear film instability with short tear film breakup time (TAZ / BUT) followed by
faster evaporation of the tear water (hyper-evaporation) with subsequent
so-called "Evaporative Dry Eye"
increased osmolarity (hyperosmolarity) of the remaining tear film
when the tear water evaporates, the dissolved substances (proteins, salts) remain and their concentration in the remaining tears increases (please see animated figure).
this is also an inflammatory stimulus .
Blinking disorder => disruption of tear film spreading ... leads to
Tear fluid alone is not sufficient for a tear film because only the normal and sufficiently frequent blinking movement of the eyelids creates the necessary film from the tear fluid.
A disorder of the eyelids themselves or the normal blinking of the eyes therefore causes a tear film disorder or can contribute to it.
Consequences are, e.g.
disruption of tear film spread
increased eyelid friction on the eyeball
chronic mechanical irritation
this is an inflammatory stimulus
Mucin deficiency ... leads to
Wetting problems
Unstable tear film, short tear film break-up time (BUT)
possibly also responsible for patients with very short BUT drye eye
'dry spots' in the tear film
increased mechanical friction and leads to chronic mechanical irritation of the epithelial cells
=> this is an inflammatory stimulus
Mucin deficiency occurs when the fine structure of the cellular surface, including the membrane-bound mucins on the microvilli and the soluble mucins of the goblet cells are damaged by:
topical damage (mechanical or chemical) in the case of disorders of the tear film - this is the typical course in the dry eye ... or by ...
Systemic damage, for example due to severe vitamin A deficiency or chronic inflammatory diseases that also involve the surface of the eye.
SURFACE TISSUE DAMAGE occurs as a consequence of tear film deficiency
The main pathogenetic factors of tear film disturbance (hyper-osmolarity and chronic mechanical irritation) lead to chronic damage to the tissue surface .
Chronic damage to the cellular surface induces
chronic inflammation, which ultimately leads to
degenerative tissue remodeling with
increasing loss of function.
Degenerative Tissue Remodeling and Loss of Function occurs in chronic tissue wounding
The chronic surface damage in dry eye affects first the epithelium, and has several downstream consequences, that act as secondary pathogenetic factors in the disease process.
These are interrelated, mutually reinforce each other and drive the disease in a pathological cascade if they are not treated by timely and effective therapy:
Damage to the fine surface structure :
the number of goblet cells on the conjunctiva decreases and squamous metaplasia develops.
this reduces the ability to bind the aqueous tears to the surface ('wettability') .
=> Reinforcement of tissue damage to the surface of the cornea and the conjunctiva (image).
Activation of cells of the surface epithelium .
=> creates an inflammation.
the cells form inflammation mediators (cytokines and chemokines) such as interferon gamma (IFN-g), tumor necrosis factor alpha (TNF). These expand the inflammation and make it worse.
Abnormal cell differentiation and angiogenesis
Chronic inflammation
Chronic friction and increased osmolarity of the tear film are inflammatory stimuli.
Since Risk Factors for a Dry Eye typically occur chronically the resulting tissue irritation cannot be eliminated by the inflammatory reaction.
Therefore, also the inflammatory tissue response becomes chronic and a progression occurs from subclinical to clinical inflammation
The inflammatory response is a response of the cells to harmful stimuli /adverse events/ noxae that threaten their integrity and function.
Inflammation is a very old protective mechanism for practically all cells and tissues of the body, especially against infections with bacteria and other microorganisms.
Typical 'side effects' of inflammatory reactions are further damage to the body's own tissue. This is accepted by the tissue as 'collateral damage' with the intention of eliminating the noxious substances as effectively as possible. In case of infections, inflammation is often effective against the pathogens. With chronic (mechanical and chemical) trauma in dry eye, this cannot work. The result is a senseless tissue damage that continues.
Immunomodulated inflammation
Chronic inflammation disturbs the normal immune tolerance of the body and therefore an immune-modulated inflammation can arise, which is modulated by T-lymphocytes.
This type of inflammation is very powerful and can lead to severe chronic inflammation with significant damage.
This finding of immune modulated inflammation in Dry Eye Disease is the basis for the use of anti-inflammatory medication, for example with lymphocyte inhibitors (such as the calcineurin inhibitor cyclosporin A, CsA) in the dry eye
The inflammatory reactions that occur drive self-reinforcing control loops of the disease exacerbation (Vicious Circles) and are an important reinforcement mechanism of the dry eye.
SYNOPSIS of the Pathophysiology in Dry Eye Disease
In the synopsis (see animation) the basic causal factors lead :
Disorder of the glandular tissue and / or
Eyelid disorder
to a disturbance of the tear film and thus the constant moistening. This triggers the two primary pathologies :
Tear film deficiency and
Tissue damage
The primary pathologies are governed and promoted by cascades of secondary pathogenetic factors . These can be collected as clinical findings and serve
Diagnostics and
staging
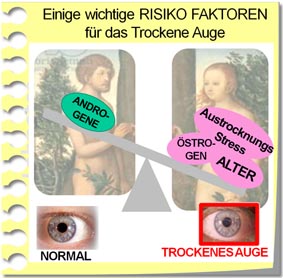
Risk factors
Various influencing factors inside and outside of the body can have a negative effect on the basic functional complexes of the surface of the eye or on the tear film. Therefore they represent risk factors and can promote the development and worsening of a dry eye.
The influence of various risk factors must be considered when assessing the development of the disease. This can help to identify the appropriate therapy options for an individual patient.
Important risk factors
Disorders of the body's regulatory systems that control the surface of the eye (such as the nervous , endocrine, and immune systems )
Internal risk factors, such as age, gender, chronic illnesses, medication or drinking amount and diet, can have a negative impact on the tissues of the ocular surface.
these include, for example, decreasing aqueous tear secretion with increasing age, increasing cornification at the edge of the eyelid, increasing tendency to eyelid deformities (entropion, ectropion), often decreasing drinking volume and a poor diet, etc.
External risk factors in the environment dry out the tear fluid and the tear film. These include, for example, drafts, dryness, dusts in the air, rare blinking or wearing contact lenses. An accumulation of such risk factors occurs in computer work environments in the office. In this context, the dry eye is known as “office eye”.
Iatrogenic dry eye
Various medications can favor dry eyes
Often underestimated internal risk factors for a dry eye are, in addition to chronic systemic diseases, various medications for the therapy of such disease.
Drugs are of negative influence for the dry eye if they change the inner milieu of the body in such a way that the production of components of the tears is disturbed or if the surface of the eye is directly changed.
Dry eye conditions that are negatively influenced by medical treatments of any kind are termed ´ Iatrogenic dry eye ´. In the current TFOS DEWS II Report (2017) a special chapter was devoted to the iatrogenic dry eye. Further details can be found in a current German-language review on the dry eye.
Many classes of medication have long been known to carry dry eyes. These include, for example
Antihypertensive drugs, such as beta blockers
some anti-cholinergics like
Anti-histamines
various antiarrhythmics
various bronchodilatants
various anti-depressants, sedatives
some anti-Parkinson medication
some pain relievers (canabinoids, opioids)
Hormones (eg estrogens, anti-androgens)
If it is suspected that a medication could promote or worsen a dry eye, the necessary desired effect must always be weighed against possible undesirable effects in order not to endanger health. Medications prescribed by a doctor should not be discontinued on your own !
Preservatives in eye drops can damage the cell surface
Preservatives in eye drops are among the external risk factors. They are still in many eye drops and can cause direct damage to the surface of the eye.
Preservatives in eye drops are substances that effectively kill germs of different kinds … but, as a side-effect, they can often also effectively kill the body’s own cells.
Especially if eye drops have to be administered chronically and frequently (such as tear substitutes or anti-glaucomatous eye drops), the preservatives contained can damage the tissue and thus the stability of the tear film.
However, a possible negative influence depends on the specific preservative and the dosage.
If it is suspected that a medication may promote or worsen a dry eye, the necessary desired effect must always be weighed against possible undesirable effects in order not to endanger health. Medications prescribed by a doctor should not be discontinued on your own!
Unfortunately, the Dry Eye tends to worsen without timely and effective therapy
The complex pathological changes in dry eye have a tendency to influence each other negatively and thereby reinforce the disease process. This is also called self-reinforcing vicious circles.
It leads to a progression in the severity of the disease if timely and effective therapy is not carried out.
The two primary dry eye pathologies, as explained above,
tear film deficiency and
tissue damage
=> both of these damage the glands of the eye (tear glands and meibomian glands) as well as the goblet cell glands in the conjunctiva and thus the mucin production and wettability of the surface.
Ocular surface damage induces
disorder of the sensory nerves on the surface with subsequent
disruption of neural autoregulation of secretion and blinking
disorder of the eyelid margin due to chronic blepharitis
=> these secondary pathogenetic factors of gland damage drive large ´ pathological carousels ´, which then intensify the primary pathologies of tear film disorder and tissue damage.
Many self-reinforcing loops that affect each other come together in the pathophysiology of dry eye. This creates a rather complex interaction of various disease factors (please see figure). This explains why dry eye therapy is still a challenge for both patients and doctors.
Self-reinforcing Vicious Circles of disease aggravation - numerous and different
Contrary to the assumption that in the pathophysiology of the dry eye ´ there is only one ´self-reinforcing vicious circle´ for aggravation of the disease, there are in fact many and different ones that are inter-related.
Against the assumption of a single self-reinforcing control loop, there is also the argument that a therapy could then be applied to any pathophysiological factor and would still always be successful. This is not confirmed by decades of experience in dry eye therapy.
The vicious circles are partially reinforced by inflammatory mechanisms, some of them, however, also work without inflammation.
A typical feature of an advanced stage of dry eye disease is the development of numerous different Vicious Circles, for example:
A lack of tears leads to tissue damage of the surface - and this in turn worsens the wetting and increases the triggering lack of tears.
Surface damage induces inflammatory reactions and this can intensify the triggering damage
Surface damage disrupts the sensory innervation from the surface of the eye. This disrupts neural autoregulation for secretion, leads to a lack of tears and thus increases the triggering surface damage.
etc.
The progression of the disease is even accelerated by immune-modulated inflammatory reactions. This can result in:
Degenerative remodeling of the tissue and
Loss of function of the surface of the eye
Typical SYMPTOMS
Damage to the dry eye leads to some typical SYMPTOMS
A detailed description of the symptoms can be found in the chapter “More information”
In summary, typical dry eye symptoms are based on dryness, irritation / irritation, and pain .
Initially, especially in the elderly, eye irritation may occasionally lead to increased lacrimation / lacrimation and wet eye .
Furthermore, the optical consequences of the disturbance of the normally uniform tear film are noticed as: deterioration of visual acuity / blurred vision / unstable vision.
It is typical of the dry eye that the subjective symptoms do not always exactly match the clinical findings .
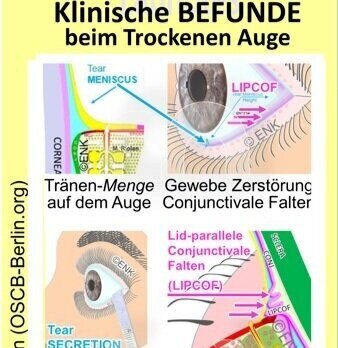
TYPICAL FINDINGS
=> You can find a short overview of typical conditions with dry eyes => HERE
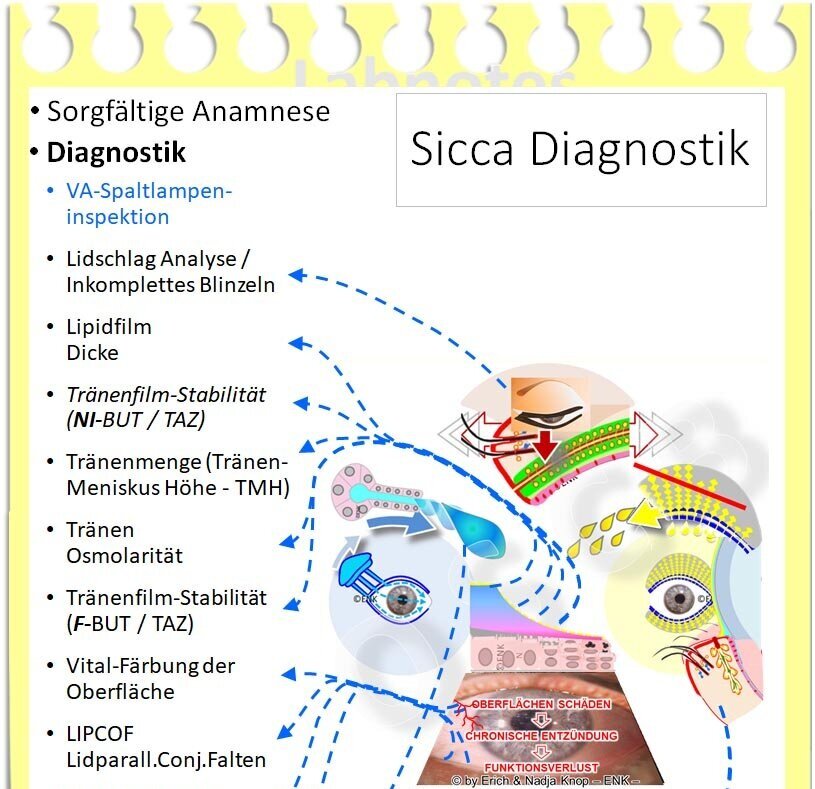
Diagnostic tests
=> You can find a brief overview of pioneering DIAGNOSTIC TESTS in the dry eye => HERE
SEVERITY
For the dry eye, a rather general division into 4 levels of severity has prevailed, ranging from easy to moderate and difficult to very difficult . Ultimately, the decisive factor is the extent of the surface damage that occurs in vital staining.
However, there is currently no generally accepted definition for the exact classification of the degrees of severity according to clinical findings.
For the meibomian gland dysfunction there is also a blockage of the glands, which ( still ) runs without symptoms and therefore has the severity level "0".
In contrast, a dry eye is by definition always symptomatic and the severity classification therefore begins with “° 1” / “easy”.
The consensus reports of the international “Tear Film and Ocular Surface” (TFOS, www.tearfilm.org ) have a certain level of acceptance.
In the TFOS “Dry Eye Workshop Report” (DEWS) from 2007, an exact severity classification was given based on numerous criteria
In the TFOS “Dry Eye Workshop Report II” (DEWS II) from 2017, such a small-scale definition receded in favor of more general considerations. There are some important parameters classified in stages, such as severity of the evaporative disorder, severity of tears and surface damage.
There is a severity classification according to the height of the tear meniscus is suggested:
0.2mm: mild
0.1 mm: moderate
0 mm: heavy
Evidence of a dry eye
No single criterion is certainly sufficient for reliable grading of the dry eye .
Both with the tear film parameters , which can often be quantitatively evaluated today ( lipid layer thickness , instability / BUT , tear meniscus , osmolarity ) as well as with the gland parameters ( aqueous secretion / Schirmer-1 test , oil secretion / diagnostic expression , meibography ) individual findings can not provide reliable evidence of dry eye.
A lack of, for example, watery tear secretion, even if it is very pronounced (less than 1 mm), cannot be reliably demonstrated by a severe dry eye. A practically dry umbrella test strip should perhaps first lead to the suspicion that this was carried out incorrectly, eg if the strip did not reach far enough into the lower fornix. Isolated deviations in the thickness of the lipid layer on the tear film or in the osmolarity are also an indication but not a reliable proof of a dry eye.
Of course, a consistent moderate to severe deficiency of various factors such as watery tear secretion, oil production, tear meniscus and tear stability makes dry eyes increasingly likely.
Practical clinical severity classification
The most reliable evidence of an effectively “dry” eye , ie symptomatic surface damage with tear film disorder, is the tissue damage that has already occurred:
this is typically caused by a previous chronic tear film disorder.
Occasionally there may also be primary chronic tissue damage , which inevitably leads to a tear film disorder.
Tissue damage is typically demonstrated as vital staining in the sense of superficial punctate keratitis (KSP).
The extent of the vital staining also gives a reliable indication of the severity of the dry eye .
If the vital staining is evaluated according to the established Oxford scheme , then there is a division into the 4 levels mentioned, from easy to moderate and difficult to very difficult .
There is an advanced level 5 for even more difficult findings, but this is of no essential importance for practical clinical work.
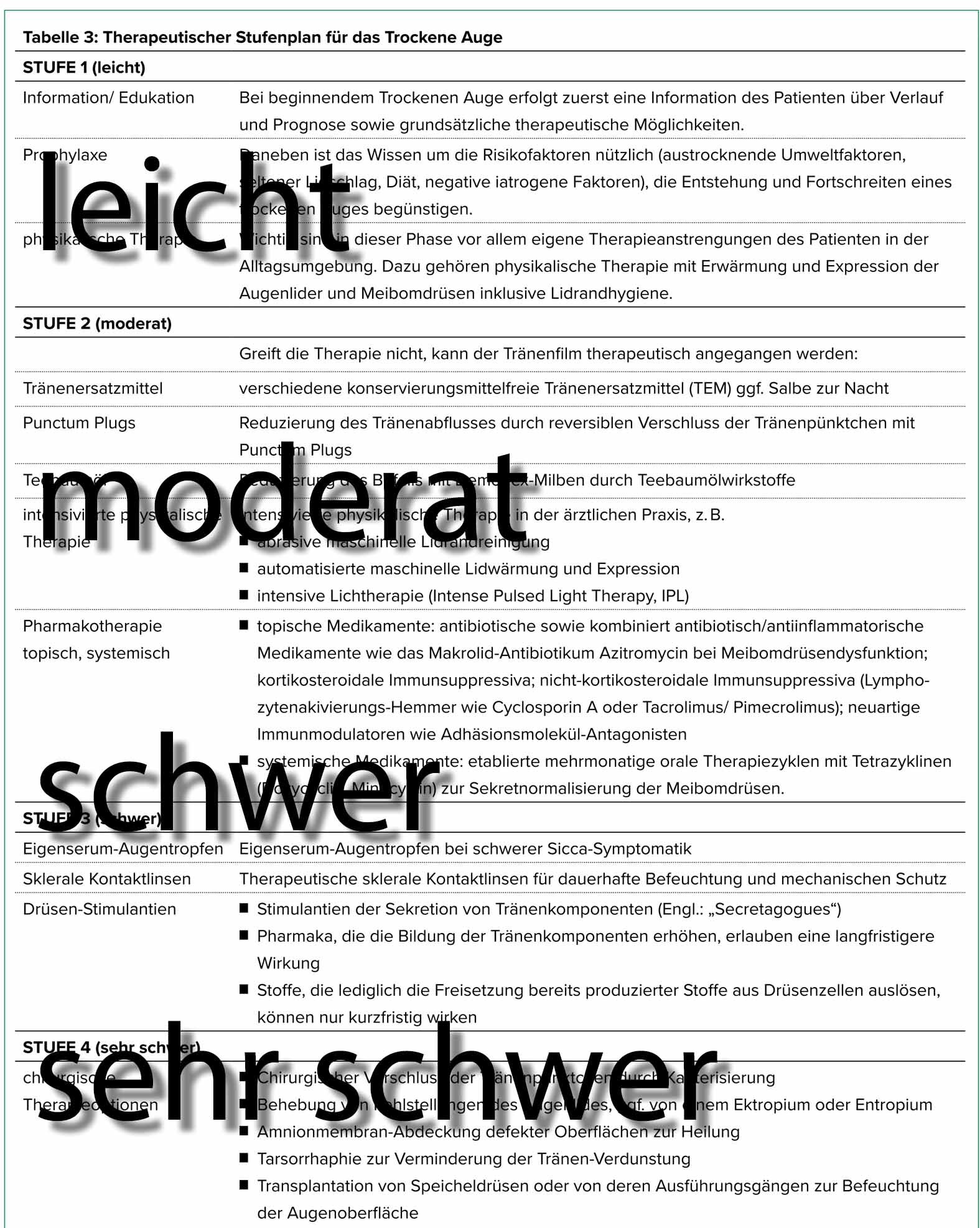
THERAPY
=> You can find a short overview of the established step therapy for dry eye => HERE
=> You can find basic considerations for various therapy options => HERE
Continue to chapter