Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT ]
Quick GLIMPSE
The ´ PATIENTS´ Page ´ on Dry Eye Disease
… will not dig too deep
but will explain interesting facts ... generally understandable !
Moisture comes from tears and is produced by the eye glands.
The tear fluid must be distributed to the thin tear film on the eye by the blinking movement of the eyelids ... to make the moisture permanent - always and everywhere ... and to allow perfect visual acuity.
Oil from the Meibom oil glands in the eyelids ensures that the tear film remains stable for longer.
If one of these conditions is disturbed, it can lead to dry eyes. They are based on a disturbance of wetting with subsequent damage to the surface tissue.
The lack of tears is usually caused by increased evaporation of the watery tears. This in turn is caused by a lack of oil on the tear film when the eyelid oil glands are blocked.
Dry eyes are promoted by numerous negative risk factors, which are partly in the body and partly in the environment. This opens up many possibilities for prevention, improvement and treatment of the disease.
Contact lenses can contribute to dry eyes ... but speciality contact lenses can in selected cases also help with severe dry eyes
Please select a TOPIC of your interest by clicking on an image
- or just follow the presentation on this page ... which is perhaps the most informative
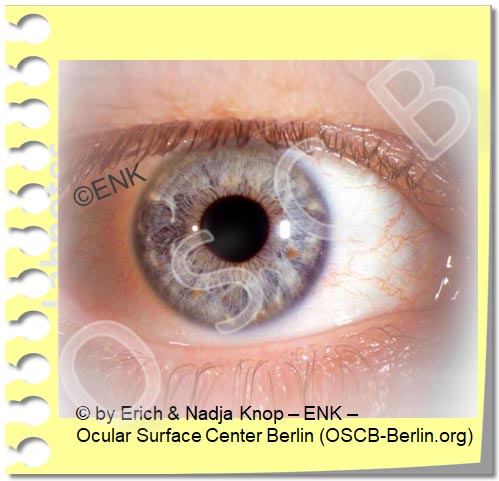
The surface of the eye
The ocular surface ... is the moist frontal part of the eye
It mainly consists of the clear cornea in the middle and the supporting tissue of the conjunctiva around it, which actually forms most of the ocular surface tissue (please see animated image).
The ocular glands and their secretions (tears) as well as the eyelids that spread the tears into the tear film are certainly also part of the ocular surface.
The cornea
is the clear tissue in the middle
it serves for the transmission and refraction of light
even though it may remind of a simple piece of ´plastic´ it is in fact a very delicate and highly specialized tissue that needs careful attention !
The conjunctiva
covers the eyeball from the front, where it lies on the hard eye wall (sclera),
then turns over and covers the eyelids from behind
thereby it forms the conjunctival sac
occasionally, foreign objects can get into the conjunctival sac (which is very irritating) and are then best rinsed out.
is the main support tissue for the cornea and helps to keep the cornea moist etc.
contains the blood vessels that are seen on the eye and can be moved with the delicate flexible conjunctival tissue
when the eye is irritated the conjunctival vessels fill up and cause the typical reddening.
The gloss on the surface of the eyes is created by moisture of the tear film, which ensures that the mucous membrane remains constantly moist - even with opened eyelids.
The tears consists of the fluid secretions from the various glands, that are somewhat hidden and also belong to the ocular surface.
The eyelids protect the moist mucous membrane and distribute the tear fluid into the tear film.
=> here you will find more in-depth information about the surface of the eye.
The surface of the eye ... allows the first steps of Vision
The surface of the eye is that part of the eye through which the light enters.
Only then can the light trigger stimuli on the retina in the back of the eye, which can later be processed into an image of the outside world in the ' curious' brain.
Without a healthy eye surface, all functions of the visual process that are further back and later are ultimately relatively meaningless for vision.
Tears - the magic juice that keeps the ocular surface healthy and going
Tears are the ´magic juice´ that serves for many, many, many purposes the ocular surface.
They are produced by different glands and consist of different substances. Tears also contain some substances from the blood.
The function of tears does not only serve for wetting of the tissue surface but also maintains e.g.:
lubrication and thus reduction of mechanical friction
regulation of growth, regeneration and wound healing of the tissue
protection against infection
oxygen transmission
… and many more functions
Wetting is probably the most obvious function of the tears and dry eye disease is based on a wetting deficiency. Therefore, (mainly aqueous) tear supplements have occurred as the most obvious from of therapy.
The moisture of the tears comes from the glands of the eye
The tear fluid is produced by several glands.
Three different types of glands are needed because the tear film on the eye is made up of three different main types of substances:
Water ... is the main part of the tears and comes from the lacrimal gland behind the upper eyelid at the outer top of the eye socket. Several small accessory lacrimal glands contribute smaller amounts of fluid.
Oil ... from the meibomian glands can reduce the evaporation of the water. Oil forms a thin layer on the surface of the tear film. The meibomian glands are elongated strands in the eyelids, They can be seen at the inside of the lower lid when it is slightly everted.
Mucus (a slimy substance composed of mucin molecules) ... mainly comes from individual small goblet cells that are distributed along the conjunctival sac (see pink dots in the figure). The mucus is needed to bind the water of the tears to the cell surface.
The various glandular products are arranged in layers in the tear film on the eye.
Tears flow along the surface of the eye
Tears are produced by the various glands on the surface of the eye.
Most of the volume consists of water and comes from the lacrimal gland, that is located at the outer upper aspect of the eye socket behind the upper eyelid.
From there, the tears enter the conjunctival sac. The tears flow towards the nasal side of the eye. This occurs behind the eyelids and along the lid margin in the lacrimal strip (tear meniscus).
Through the blink movement of the eyelids the tears are spread into the thin tear film over the visible frontal part of the eye and keep the tissue moist.
On the nose side, the ´used´ tears are then sucked up by small holes (lacrimal puncta). One punctum each occurs on the nasal side of the upper and lower eyelids and they dip into the lacrimal strip.
Tears reach the nose through the draining tear ducts (please see animated figure). When larger quantities of tears get there, e.g. when crying, they can run into the throat, where we can notice their salty taste.
Alterations of eyelids or a blockade of the nasal outflow, often with bacterial infection, can both cause a ´wet eye´ with overflow of tears over the edge of the eyelid.
The meibomian glands are of particular importance for the surface of the eye
The meibomian glands in the eyelids produce oil for the tear film
Meibom oil protects the tear water from evaporation .
The meibomian glands form long strands in the eyelids. They produce lipids/fats that are liquid at body temperature and thus form an oil.
Meibomian glands are of particular importance for the health of the ocular surface because their oil retards the evaporation of the watery tears.
In the dry environment we live in, the watery tears evaporate faster from the surface of the eye than the lacrimal gland can produce them. We therefore need an oil layer on the surface of the tear film to sufficiently inhibit evaporation.
A lack of oil on the tear film and/or environmental factors that increase evaporation … will both favour a dry eye condition.
A lack of oil on the tear film is the main primary cause for dry eye disease, particularly in elderly individuals.
Desiccating environmental factors often occur in office environments and cause dry eyes in many younger individuals.
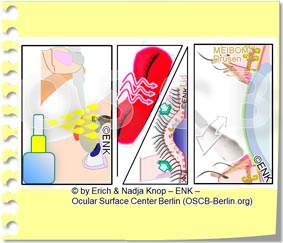
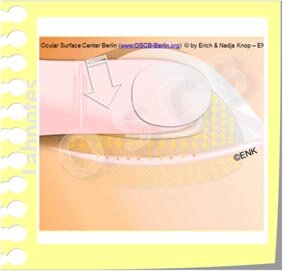
The blink movement of the eyelids ensures the squeezing of the meibomian glands
The blink of the eyelids ensures that the meibomian glands are squeezed out: the meibomian glands form the oil through piles of glandular cells in rounded end pieces (“secretion” at the bottom left of the figure). The glandular cells lie deep in the eyelid and fill the duct system of the glands with lipid secretum (arrows). The light pressure of the eyelid muscles, upon the blink of the eyelids, pushes oil droplets out of the gland opening at the edge of the eyelid (“Dellivery”).
The power of muscle contraction when blinking contributes to squeezing meibom oil out of the glands, increasing the thickness of the oil layer on the tear film
Rarely blinking is therefore an important cause of an oil deficiency on the tear film and may be a co-factor for the onset of meibomian gland dysfunction (MDD).
Deliberate, forceful blinking helps, according to studies, as an easy way to increase the oil layer on the tear film and thus increase the stability of the tear film and avoid or improve a dry eye.
The eye surface must be constantly moist
The surface of our eyes is a mucous membrane. It is constructed in such a way that it has to be permanently moist - ´everywhere´ - so that it stays healthy and that the cornea, the clear window of the eye, remains really clear.
This moisture is produced by the glands on the surface of the eye and is known as tears *.
Since we live in a dry environment with an air atmosphere, it is very difficult for the eye to maintain this small, artificial, moist "ecological niche" on the surface of the eye - "Always and everywhere"!
* In addition to keeping the ocular surface moist, we can also use the tears to convey the emotional signal to our fellow human beings that we are particularly sad ... or particularly happy - Hmmm ... doesn't it say 'tears don't lie'? ... but with that we leave the sure ground of science and therefore do not pursue it further!
The eyelids and blinking are just as important as the tears
A sufficiently frequent and complete blinking is necessary for an even and stable tear film.
a blink mainly moves the upper eyelid down, and wipes over the cornea and conjunctiva
when wiping down the ´old´ tear film is ´ cleared away´ (into the lacrimal tear strip) - and the tears are sucked into the lacrimal puncta and transported to the nose.
a new tear film is spread out when the upper eyelid is opened
The tear film is a ´trick´ of the eye for moisture and vision at the same time
Moisture "always and everywhere" presents a problem to the surface of the eye, or, to put it more nicely, a challenge :
Only when the eyelids are open can light enter the eye ... but then the surface of the important cornea would begin to dry out immediately. Therefore, the eye has a ' trick ' access:
A thin layer of tear water - called the " tear film " - is formed, which is thick enough to keep the cell surface moist , but thin enough not to disturb the entry of the light!
Another important effect of the tear film is that it fills all ´unevenness´ of the surface and thus creates a perfectly smooth surface for a perfect refraction ... for a perfect visual acuity !
Since only the regular blinking of the eyelids can produce a stable tear film, the eyelids and their blinking are just as important as the production of the tear fluid.
The Tear FILM is the solution for all 'Problems' on the ocular surface ... and for the SEEING
The tears are transformed into the important thin tear film.
This happens through the orderly blinking, i.e. the wiping movement of the eyelids over the surface of the eyeball.
Only by blinking and the special composition and arrangement in layers of the tear film it becomes possible to produce a very thin (about a hundredth of a millimeter) tear film.
The tear film must remain stable at least until our curious brain has a sufficient picture of what is going on in the environment. The tear film should remain stable for at least 10 seconds until it breaks up.
The ´break-up´ of the tear film is then the stimulus to trigger a new blink of an eye, which spreads a new tear film.
The tear film forms a thin and even coating on the surface of the eye
View into the tear film
The surface of the ocular cells is covered with a thin, even coating of tear fluid - the tear film. For the adhesion of the watery tears serve water-binding mucilages (mucin molecules, in the figure indicated as pink fibers). Some are attached to the cells and others are dissolved as a gel in the water of tears. In addition, the cells have numerous finger-like extensions that enlarge the surface and thereby improve the adhesion. If the normal cell surface is damaged, the binding of the tear film to the tissue surface is reduced and it breaks up quickly.
The tear film is arranged in layers
The tear film coating is distributed on the surface in a layer-like stucture by the eyelid blink movement of the lids. The layers are not sharply separated but instead mixed to a certain extent. Each layer of the tear film consists mainly of the secretions of one type of gland.
the bottom layer is formed from the mucilage (mucin molecules, shown as pink ribbons in the figure). They bind the watery tears to the cell surface and thus maintain wettability of the tissue surface.
the middle main layer of the tear film consists of the water of the tear gland, which together with soluble mucilage forms a water-mucin gel . This is used for ´ lubrication ´, that is, to reduce the friction between the eyelid and eyeball during frequent eye flaps. In addition, the tears contain numerous important substances for keeping the tissue healthy.
the surface layer is very thin and consits of the oil (yellow in the picture) of the meibomian glands, which are located in the eyelids. The main function of the lipids in the oily layer is to reduce the evaporation of the watery tears. If oil is missing, evaporation increases and dry eye can easily develop.
Only a thin and even tear film allows perfect visual acuity
An intact, thin and even tear film is not just for moistening of the ocular surface.
It is also the prerequisite for perfect refraction and therefore good visual acuity.
Tear film disorders typically lead to decreased or fluctuating visual acuity
In principle, everything is already said:
The basic requirement for health and visual acuity is a stable tear film that is created by the
Production / secretion of tears through the eye glands and the
Formation / spreading of the tear film by eyelid blinking
... and if the conditions for keeping moist are disturbed or the tear film dries out due to external factors - then there is a dry eye !
DRY-EYE-DISEASE
… after the moisture is gone
When there is no (sufficiently) stable tear film, the eye will dry up !
How does a dry eye show up?
Blurred Vision and Eye Irritation occur when the tear film breaks-up
Development of a ´dry spot´in the tear film due to tear film deficiency
The tear film only has a limited 'durability' of approx. 10-20 seconds - this is called ´tear film stability'.
Therefore, the blink of the eye must be repeated frequently - about every 10 seconds or about 5-10 times a minute - to spread a new tear film with every blink.
If the tear film is not renewed in time, it locally becomes thinner and breaks-up (see animated figure). The resulting ´dry spot in the tear film´ has 2 consequences:
the refraction of light becomes irregular and the visual acuity becomes unstable or blurred. This is often an early indication of a dry eye.
the tissue begins to dry out immediately.
this triggers irritation of the nerve fibers located there and thus induces a new blink or increased tear flow.
repeated irritation leads to symptoms of eye irritation that are known to all patients.
chronic irritation can also lead to pain and can possibly develop into a pain syndrome
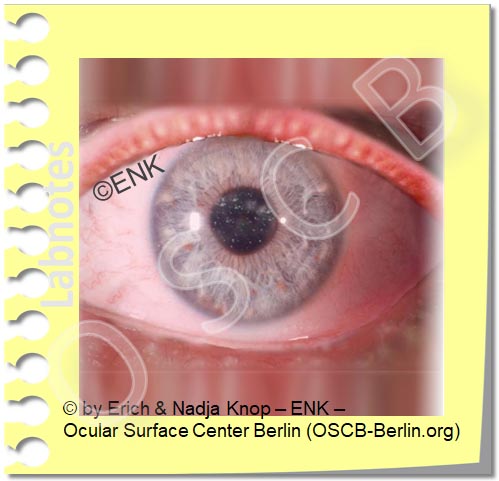
Damage to the tissue surface results from disorders of the tear film
When the tear water evaporates (blue wavy arrows), the salts and proteins (grey circles in the liquid) remain and cause a more concentrated "salty" composition of the remaining tears, called "hyperosmolarity". Hyperosmolarity, similar to increased mechanical friction, irritates eye tissue and cells. This leads to damage and inflammation in dry eye disease.
All disorders of the tear film lead to damage to the tissue on the surface of the eye.
First the water-binding layer of mucus (indicated pink in the figure) at the bottom of the tear film is damaged and later the numerous small finger-like cell extensions are damage or lost. Both are important for the ability of the surface to bind water.
When the wetting is thereby disturbed, the tear film becomes unstable and breaks-up easily. This creates gaps/ holes in the tear film, termed as dry spots.
Dry spots in the tear film increase the mechanical friction during movements between the eyeball and eyelid, e.g. during regular eyelid strokes. This causes further damage.
If evaporation of the aqueous tears increases the salt concentration in the remaining tears (increased osmolarity/hyperosmolarity), this leads to damage through dehydration and cell shrinkage (see animated figure).
The osmolarity of the tear film can nowadays be measured relatively easy.
Increased mechanical friction and increased salinity of the tears (hyperosmolarity) puts the cells into an 'alarm state' and can trigger further reactions such as an inflammatory reaction - an important reinforcement mechanism in dry eye.
Later there are gaps in the cell layer and the tissue shows degenative remodelling leading to a loss of function.
Rarely, the tissue at the surface of the eye is damaged first, with a later secondary disorder of the tear film and moistening.
Tear film disorder leads to tissue damage, irritation, inflammation and pain
Tear film deficiency with damage to the surface of the eye and irritation of nerve fibers triggers the typical findings of Dry Eye Disease:
various complaints of eye irritation
increased blood flow on the ocular surface that leads to reddening
often blurred vision with or without wet eyes
sticky eyelids due to increased production of mucus and other secretum
irritation of nerve fibers is triggered by surface damage
Nerve fibers are particularly numerous on the surface of the eye, which is why it is so sensitive to touch, foreign bodies and dryness.
triggers irritation of the nerve fibers and thus induces a new blink or increased tear flow.
repeated irritation leads to symptoms of eye irritation that are known to all patients.
chronic irritation can also lead to pain and can possibly develop into a pain syndrome
Inflammatory reactions can make the process worse.
Oil Deficiency as the most common primary cause
According to the current state of scientific knowledge, the vast majority, ie four out of five patients with a dry eye, do not have a primary lack of tear water, as one might suspect, but a causal lack of OIL on the tear film.
Lack of oil is caused by meibomian gland dysfunction (MDD) then leads to increased evaporation with decreasing stability of the tear film ... and usually later lack of water .
Therefore, it does not seem to make much sense to use products that do not contain lipids in most dry eye patients today.
It is also possible to use additions of other substances which replace the action of the lipids, or even only lipids, for example as a liposome spray.
In other words, lipids or other substances with a comparable effect should now be part of a typical tear supplement therapy / tear substitute for the dry eye.
A lack of oil is typically caused by constipation of the meibomian glands in the eyelids
The occurring lack of oil is typically due to a malfunction of the meibomian glands, the meibomian gland dysfunction ( MDD ).
It usually consists of constipation of the many small oil-producing meibomian glands in the eyelids.
A diagnosis of the glands can be used to check whether the meibomian glands are blocked .
Gland obstruction comes from oil and dander
The glandular openings on the edge of the lid are blocked by thickened oil and increased cornification and desquamation of the glandular tissue and skin on the edge of the lid.
This is the most common cause of Dry Eyes.
The thickened oil is no longer clear and fluid, but becomes whitish to yellowish and viscous. The thicker it gets, the harder it is to squeeze out.
Oil and dander can form a plug in the gland opening on the edge of the lid.
Thickened secretion builds up in the glands and becomes increasingly viscous and harder.
Therapy : Therefore, a frequently performed treatment consists in heating the eyelids with the glands in them sufficiently to liquefy the fat and to be able to massage it out.
Obstruction of the meibomian glands leads to oil deficiency and unnoticed glandular destruction
2 Causes
The meibomian gland dysfunction (MDD) with constipation of the glands typically has two causes :
Thickening of the oil in the duct system in the glands
Horny gland opening
=> Both together lead to the blockage of the gland opening ( picture ).
2 Consequences:
The obstruction of the Meibominan glands has 2 main Consequences (please see Image):
Dry Eyes because of the oil deficiency on the tear film and increase evaporation of the tear water, termed as an ´Evaporative Dry Eye´)
progressive self-destruction of the gland tissue inside the eyelids due to the increased pressure inside the blocked glands
Therapy:
Therefore it is important
to treat not only the resulting oil deficiency in Dry Eye Disease, e.g. by Tear Supplements
but also to address the causative gland blockade , e.g. by Physical EyeLid Therapie with warming, gland expression and EyeLid Hygiene
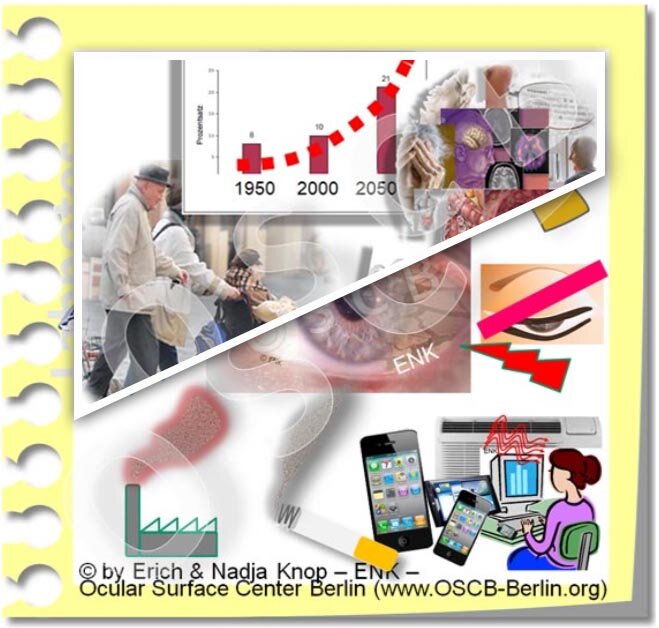
Risk Factors
Various influencing factors damage the tear film
The production and maintenance of the tear film is very complex in our dry environment, and it is therefore very susceptible to failure .
The tear film is dependent on many and very different influencing factors that can change the tear film in any way positively or negatively.
All negative factors are risk factors - sooner or later, and especially if they become chronic, they can lead to a dry eye.
The large number of risk factors, which may seem unrelated at first glance, often give the impression that the dry eye is a " tricky disease " - although the connections are actually quite simple.
External risk factors
Environmental Factors
In everyday life, external environmental factors are particularly important as risk factors. These are all influences that can disturb and damage the finished tear film on the eyes, e.g. smoke, dust, preservatives in eye drops, contact lenses.
Drying out environmental influences such as warm and dry air, blowers in cars or in air conditioning systems, etc. are particularly common here . Therefore, a dry eye generally occurs more frequently in dry or moving room air from air conditioning systems and during the heating season in winter. Here simple ' home remedies ' can already prevent and improve.
Eye Drops
Drugs that reach the eye surface from outside as eye drops are, of course, also external risk factors. Depending on the active ingredient used, they can, under certain circumstances, damage the tissue of the eye surface and contribute to dry eyes, especially if the eye drops are applied permanently.
This is particularly important if eye drops contain preservatives. Preservatives are usually relatively aggressive substances which kill microbes and thus should keep the eye drops germ-free. However, they can also attack the cells of the ocular surface and thus damage the tissue on the surface of the eye and thus contribute to dry eyes. The more often such eye drops are used and the more aggressive a preservative they contain, the greater the risk of possible damage.
For more information, please consult your eye doctor.
Internal risk factors
Internal risk factors arise from malfunctions in our internal regulatory systems (nervous system, hormone system, immune system) and from systemic diseases that have a negative impact on eye health and tears.
increased age and chronic diseases
The normal aging processes in the body also affect the functionality of the eye.
This leads to, for example
decreased watery tear production
increased cornification of the skin on the edge of the eyelid with an increased tendency to blockage of the meibomian glands
Increased tendency to change the shape of the eyelids with disturbance of the formation of a stable tear film
Increased tendency to chronic systemic diseases , such as cardiovascular diseases (e.g. high blood pressure), metabolic diseases (e.g. diabetes mell., thyroid disorders), chronic inflammation (e.g. rheumatic diseases).
Even drugs that chronic diseases for treatment are used, may have a negative impact on the health of the eye and convey a dry eye.
Hormones are another important risk factor and this also affects the changes in hormones with increasing age.
The sex hormones are of particular importance , among other things because they act on the glandular tissues. Men and women have both male sex hormones (androgens) and female sex hormones (estrogens, progestogens) - but in different amounts.
In general, and very much simplified, male sex hormones are considered to be rather beneficial for the glands, tear system and surface of the eyes, while female sex hormones are considered to be rather negative. However, this also depends on age and many other factors.
The important influence of sex hormones explains why the dry eye generally occurs more often in women and increases with age in both sexes. In menopause and menopause, the frequency of dry eye increases in women - according to studies, hormone replacement therapy leads to a further increase.
... some BASIC ideas for THERAPY
What can I do ? … as a therapy for dry eye disease ?
Different inter-related factors contribute to ocular surface disease including the dry eye. These can be approached and improved by different therapy approaches:
Typically there is a deficiency of the Tear Film based on a qualitative or quantitative lack of tear components. Tear Supplementation, i.e. the addition of missing tear components, is thus the most frequently used therapy option.
The main reason for dry eye disease is a lack of oil due to obstruction of the Meibomian glands. This allows a semi-causative therapy to improve the gland function. A ´physical lid therapy´ with heat and lid massage can be performed at home by the patients.
All types of dry eye disease and chronic eyelid inflammation (blepharitis) are related to the accumulation and incrustation of debris on the lid margin that leads to worsening of the condition. Therefore specific lid hygiene to clean the eyelids and a general eyelid care is useful to promote the health of the ocular surface and thus to improve dry eye disease.
TEAR SUPPLEMENTS are a cornerstone of Dry Dye therapy
In dry eye disease there is typically a deficiency of the tear film based on a deficiency in the amount or quality of tear components.
Therefore, the most common therapy is tear supplementation, i.e. the addition of (missing or insufficient) tear components.
This is often referred to as 'tear replacement' or ´artificial tears´. Unfortunately, it has not been possible at present, and for the foreseeable future, to completely replace the natural tears. The term tear supplements thus appears to be most appropriate.
An almost unmanageable number of different tear supplements is available. These are mainly eye drops, that are based on aqueous solutions and that can contain different additional active ingredients. Most of the tear supplements are available as over-the-counter products without prescription.
Physical LID MARGIN THERAPY is a basic therapy for Meibomian Gland Dysfunction (MGD)
It can improve oil deficiency and potential gland damage by reactivating the meibomian oil glands inside the eyelids
The concept of ´physical therapy´ is based on simple but effective physical techniques for the treatment of the eyelids and the meibomian glands. Heating and humidification, massage and squeezing as well as subsequent intense cleaning of the lid margin is performed.
Before any manipulation of the eyelid and eye, it is of course important to consult an ophthalmologist beforehand in order to get a qualified diagnosis and appropriate therapy suggestions to avoid injuries to the eyelid and eye ! It is also important to have the potential progress or failure of therapy followed by the eye doctor !
Dry eye disease is a chronic illness, that has typically developed over a period of years or often decades and thus it is often necessary to perform an equally consistent permanent i.e. ´chronic´ treatment. Long-term physical therapy is therefore typically necessary about once or twice daily.
The Methods of Physical Therapy can be applied in different ways (=> HERE is more information):
as BASIC Therapy at home - this will be described here below
as APPARATIVE Device-Based Therapy - this is performed in the eye doctor´s office. The application of specialized equipment is typically more effective and results in a quicker improvement of symptoms. In addition, specialized devices offer novel therapy options that are not available at home.
=> here is an Overview of all methods for the therapy of the eyelids and Meibomian glands.
Physical therapy consists of 3 steps:
1. Warming of the eyelids
if possible with moist heat for at least 10 minutes
to achieve a temperature of approx. 40 ° C inside the eyelid, i.e. also in the Meibom oil glands
serves to re-liquefy the changed and hardened oil in the meibomian glands.
according to studies, in order to reach a temperature of 40°C in the eyelid, a warm, moist compress / clean washcloth (with a temperature of approx. 45 ° C) must be used for approx. 10 minutes; (please see animated figure)
as the temperature cools down quickly, the compress/ rag must be renewed/ reheated approximately every 2 minutes
The moisture softens encrustations at the gland openings and on the edge of the lid
Commercially available Gel Masks or even electrically heated and moistened Goggles can make the laborious physical EyeLid Therapy können significantly easier.
2. Subsequent massage of the eyelids to squeeze and empty the glands
when the inspissated oil in the meibomian glands is warmed up enough, it becomes more fluid again
by gently massaging the eyelids, it can then be squeezed out of the glands
this must be done towards the open edge of the eyelid (´eyelid margin´ - see animated figure) - so:
down the upper eyelid and
upwards on the lower eyelid
in any case, as already mentioned, a chronic illness like dry eye disease with Meibominan gland dysfunction, also requires chronic therapy in order to achieve noticeable improvements.
Therefore, even a properly performed gentle eyelid massage does not necessarily always lead to visible expressed inspissated Meibom oil on the lid margin.
Still, a consistently performed physical therapy typically results in a constant improvement of the condition … constant dripping wears the stone !
... if the glandular squeezing does not achieve a sufficient improvement of gland function despite long (over months) regular and careful application, then there are further specialized procedures and devices for the therapy of Meibom gland disorders (MDD) and eyelid inflammation (Blepharitis) in the ophthalmologist's practice.
3. Eyelid margin hygiene at the end
Finally, the eyelid should be cleaned together with the eyelashes:
of the squeezed oil
of bacteria that multiply in the oil residues
of hardened lipid deposits and skin cornification on the edge of the eyelid
Cleaning consists of a mild (soap-free ) 'scrubbing' of the edge of the eyelid with a cotton swab or facial tissue to remove deposits that can promote inflammatory events:
if the deposits are more liquid-oily, a dry cotton swab can often do a good job
if the deposits are rather dry and crusted, a damp cotton swab is usually more suitable
There are also commercially available cleaning sets with solutions, typically oil-based so as not to damage the tear film lipids. Such sets already contain all the necessary things and can thus make physical therapy considerably easier. Pre-prepared sterile cleaning pads are available for daily lidcare.
In case of a chronic therapy-resistant chronic eyelid inflammation (blepharitis), an increased infestation with normal Demodex hair-mites may be considered, which are sensitive to a therapy with tea tree oil products.
Overview of the options of physical therapy
The physical therapy measures shown here have the advantage that they can usually be carried out by the patient himself in his home environment. This is the BASIC therapy for meibomian gland dysfunction (MDD) and chronic eyelid inflammation (blepharitis).
=> here you will find more information about BASIC Therapy at home
A disadvantage may seem to be that this has to be done permanently and regularly, preferably twice a day, in order to achieve a noticeable positive effect - similar to brushing your teeth - but requires a little more time.
If the basic therapy of the eyelids at home does not achieve a sufficient improvement in spite of a longer period of regular practice, there are other specialized procedures and devices for the APPARATIVE therapy of meibomian gland dysfunction (MDD) and chronic eyelid inflammation (blepharitis) in the ophthalmologist's practice.
=> here you will find more information about APPARATIVE device therapy in the medical practicebut ... the effort is worth it, because a 'happy' eyelid typically ensures a happy patient!
... or to put it in Roman form: ´ palpebra sana in corpore sano ´ - unconfirmed quotation from the famous Roman doctor Clarissimus GALEN ;-)
QUICK GLIMPSE on …
Contact lenses
Contact lenses are a fantastic optical tool with a close relationship to the surface of the eye and also to the dry eye
Contact lenses are a fantastic optical aid, with some clear optical advantages over glasses.
At the same time, they allow greater " freedom " for leisure activities, sports and social appointments.
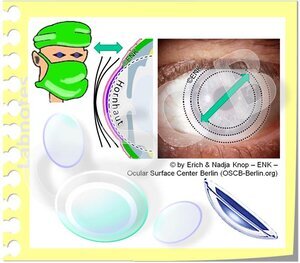
Dimensionally stable contact lenses (illustration) are relatively small and only sit on the cornea . This type of lens is particularly stable and has high optical quality. Modern lenses also have high oxygen permeability.
In the past, these lenses were made of a different material (plexiglass) and were therefore called "hard" contact lenses.
In addition to being worn normally, dimensionally stable contact lenses are also suitable for optically correcting an irregular corneal surface ( astigmatism - often called astigmatism ). Strong astigmatism can often not be completely compensated for with glasses.
Contact lenses sit in the 'middle' of the eye surface
As their name suggests, contact lenses are in direct contact with the surface of the eye.
Contact lenses are located right in the middle of the functional unit of the surface of the eye - on the eyeball and behind the lids in the conjunctival sac .
This means that they have a possible influence on all tissues and on the tear film . With every blink, for example, the back edge of the upper eyelid (illustration) must slide over the edge of the contact lens when the lid is closed. This is a common area for irritating irritation.
Contact lenses therefore have a somewhat ambiguous effect on the eye - with advantages and disadvantages.
' Soft' contact lenses (Figure), also called hydrogel lenses, are the most common type of contact lenses. This is probably due to the fact that it takes little or no time to get used to the lenses until they can be worn without discomfort and irritation.
Soft lenses are larger than dimensionally stable contact lenses and extend beyond the cornea to the conjunctiva.
Contact lenses float in the tear film on the eye ... and have increased demands on the tear film
In principle, contact lenses place higher demands on the quantity and quality of the tear film .
It is possible that someone with no signs of dryness will develop dry eye symptoms after inserting a soft hydrogel contact lens . This may be due to the fact that there was a borderline normal tear film that is no longer sufficient for a contact lens.
A typical side effect of wearing contact lenses is therefore the appearance of symptoms of dry eyes or even the development of a dry eye .
If there is already a lack of tears, contact lenses should not be worn. Permanent wetting with tear substitutes / artificial tears is also not a recommended permanent solution.
The only exception is wearing therapeutic scleral contact lenses.
Scleral contact lenses can be used to treat very severe dry eye
Although the widespread soft contact lenses can cause or worsen a dry eye, another special type of contact lens (scleral lens) can be used as a therapeutic aid in patients with severe dry eye .
Scleral contact lenses are very large and dimensionally stable. They cover the cornea with a teardrop lake and extend far beyond the conjunctiva. Underneath is the hard eye wall ( sclera ). The surface of the eyes is constantly bathed in a lacrimal lake and a heavy dry eye can be kept permanently moist.
Because scleral contact lenses span the cornea, they can also compensate for very severe irregularities in the cornea, for example when the keratoconus is disturbed .
These large lenses require a very special adjustment by an experienced contact lens specialist. It becomes clear that contact lenses are a medical device (medical device) with a direct impact on the eye , which requires careful selection, adjustment and follow-up .
The adaptation of a contact lens determines its influence on the surface of the eye:
An exact adjustment is necessary for contact lenses!
( 1 ) In order to keep possible damage to the eye to a minimum, contact lenses must always be precisely adjusted by a specialist .
If the adjustment is too flat, the contact lens is mainly on the middle of the cornea.
If the adjustment is too steep, the edge of the contact lens will rub against the conjunctiva of the eyeball.
With any type of adjustment, rubbing the edge of the contact lens on the back edge of the eyelid is inevitable due to the movement of the upper eyelid during frequent blinking (approx. 5-10 times per minute)
A well-adapted contact lens can also change when worn on the eye as well as during cleaning and storage. In addition, minor damage to the lens can occur during handling. This can lead to a changed fit on the eye and thus possibly to increased friction.
( 2 ) Contact lenses should therefore be checked by a specialist at regular intervals after the adjustment .
Contact lenses can have a negative impact on the fine structure of the surface of the eye
Although the usual adaptation principles typically aim to avoid excessive mechanical contact with the surface of the eye, contact lenses are inevitably in contact with the surface of the eye, just as their name suggests.
Contact lenses can therefore have varying degrees of mechanical and chemical influence on the surface of the eye.
This primarily concerns the interaction of the contact lens with the very sensitive central cornea and the similarly sensitive posterior edge of the lid .
The conjunctiva on the eyeball and on the back of the eyelids is less sensitive, but it is also in contact with the contact lens and therefore also exposed to a possible negative influence.
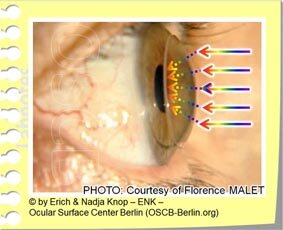
Chronic mechanical irritation of the conjunctiva can lead to squamous metaplasia
The conjunctiva / conjunctiva of the eyeball has been shown to change when wearing contact lenses . This happens in the area where the edge of the contact lens rests and rubs with every eye movement.
The epithelial cells change and the mucus cells that moisturize the surface become fewer and disappear, at least in the area in which the contact lens rubs.
The normal cubic cells of the conjunctiva are transformed into flat cells and this forms a squamous epithelium - a different type of tissue than is normally present here.
This is called squamous metaplasia (see figure). This disrupts the important wetting of the eye surface and promotes the formation or worsening of a dry eye.
Hygiene - a crucial factor when wearing contact lenses
With contact lenses there have been enormous improvements in the material quality and in the shape of the lenses in recent decades. This has led to a reduction in the frequency and severity of contact lens side effects.
However, hygiene is still a very important issue , above all ... but not only ... for inexperienced contact lens wearers.
Inadequate hygiene can lead to serious eye infections , which can endanger vision and, without immediate adequate therapy, can even lead to eye loss.
Dangerous infectious agents (bacteria, amoeba and also fungi etc.) are typically introduced through the handling of the contact lenses, either by the wearer or, for example, by contaminated water.
Therefore, contact lenses should never be treated with tap water and should not be worn while bathing or showering .
Microbes multiply in the contact lens containers or in hard-to-remove deposits (biofilm) on the contact lenses themselves.
The emergence of infections is further promoted by constant micro inevitable injuries, which by normal contact lens wear arise. These small injuries open an entrance gate for the microorganisms through the normally practically impenetrable dense surface of the eye .
Microbes are hidden in the biofilm
Bacteria and other pathogens produce a material called biofilm around them on the contact lens and in the storage container .
Biofilm is a protective layer for the bacteria that is very difficult to remove and requires thorough mechanical cleaning, for example with cleaning solution and rubbing with your fingers . In biofilm, they are not safely destroyed by disinfectant solutions either.
Contact lenses must be cleaned and disinfected thoroughly
For a thorough and safe cleaning of contact lenses and storage containers , the following is required:
(Fig. 2) mechanical cleaning
to remove
Deposits from the tear film (oil, protein, mucilage, salts)
bacterial biofilms in which bacteria hide and protect
(Fig. 3) a subsequent disinfection - bubbling peroxide solutions, for example, are proven overnight.
to kill microbes that could lead to infection
after inserting the lenses on the eye, it is very important to let the storage container dry out !
Further information on contact lens hygiene can be found => here
Disposable DAILY contact lenses have many hygienic advantages
Especially inexperienced contact lens carriers have an increased risk of eye infections.
People with a reduced immune system , such as children and the elderly, are also at greater risk from eye infections.
For soft hydrogel contact lenses are daily disposable / one-time contact lenses a good solution.
They are worn for only one day and then disposed of.
The next day, a new sterile packed contact lens is inserted. This can avoid most hygienic problems.
Daily lenses no longer need to be cleaned and stored. By avoiding these critical steps, bacterial growth is in principle greatly reduced.
Daily lenses are relatively more expensive than lenses that are worn longer (over 14 days to 1 month). However, they no longer need to invest in cleaning solutions and do not have to be laboriously cleaned daily. Both reduce the effort with this type of lens.
In terms of hygiene, daily lenses have a clear advantage and the infection rate is lowest with this type of lens.