DEEPER INSIGHT into ...
NEW DRY EYE CONCEPT
How to understand the Ocular Surface and Dry Eye Disease
After decades of intense research activities world-wide on the Ocular Surface and Dry Eye Disease a large body of results and knowledge has accumulated. Luckily this process isstill continuing and gets even faster with new technologies. This helps us to recognize more aspects of the disease process and to understand it better in order to find more efffective therapy approaches.
On the other hand, as the view on Dry Eye Disease is becoming more and more multifaceted, it often appears more complicated and the large ´picture´ of this condition becomes at times increasingly unintelligible to many people.
PATHOPHYSIOLOGY is KEY... because it refers back to the Anatomy and Function
In order to fully understand the complex disease process in Dry Eye Disease it is useful to be informed about the Ocular Surface Structure and Function as such
... because the pathophysiology of the disease process typically develops along the impairment of the physiological functions that join the organs of the anatomical unit into a functional unit.
Pathophysiology describes HOW the pathological alterations of the normal physiology lead to manifest pathology.
The BASIC FUNCTIONAL COMPLEXES of the Ocular Surface depend on its Anatomical Construction and on the Functional Collaboration ... that is dictated by the eventual aim
Along with the present construction principle of the eye, this eventual Optical Function of the Ocular Surface requires Moisture.
Therefore basic functional complexes of the Ocular Surface are there to secure that the Ocular Surface tissues can be kept constantly moist.
The BASIC FUNCTIONAL COMPLEXES are:
- Gland Tear SECRETION
- Eye LID Tear FILM FORMATION
The Ocular Surface has some requirements - one is an anatomical unit of suitable organs
In order to provide moisture, the Ocular Surface is composed of a mucous membrane including the adherent glands for the production of moisture in the form of tear fluid and a lacrimal drainage system for disposal of the "used" fluid after is has bathed the mucosa for a while.
The organs that constitute this complete Ocular Surface are an Anatomical Unit.
Another requirement is that these organs work properly together and thus constitute a FUNCTIONAL UNIT
Together with the regulatory systems that provide their maturation and their functional regulation they become a Functional Unit for the provision of moisture see also the Section ´Ocular Surface´.
Only when the regulatory systems such as the:
- nervous system
- endocrine hormonal system
- immune sysstem
work properly, they can realized a functional unit at the Ocular Surface.
Moisture means nothing when it is not equally distributed and permanently present - BLINKING is necessary
The Ocular Surface does not only consists of areas that are constantly hidden in the depth of the conjunctival sac and elsewhere, but also has areas at the anterior surface of the eye ballthat are exposed to the ambient dry air and therefore prone to desiccation- the cornea and the conjunctiva.
In order to keep the cornea and conjunctiva constantly moist (and also for refraction of incoming light) a tear film must cover these tissue even when they are exposed during the period between two blinks - the interblink period. This sets another requirement apart from tear fluid - a mechanism for spreading the tears into a tear film is necessary ... and this is the LID APPARATUS with its different accessory structures.
Eye Lid BLINKING is a highly regulated process that depends on the nervous system
A simplified scheme of the nervous system in relation to the Ocular Surface. The cranial nerves V (trigeminal) and VII (facial) maintain the reflex arcs that drive the regulation of secretion by the ocular glands and of the lid apparatus for blinking.
Since the tear film that is spread by the lid apparatus has unluckily only a limited stability of some (around 10 to 20) seconds it must be frequently renewed.
In order to do that, a servo system composed of different parts of the nervous system is necessary. It consists of
- peripheral sensors at the ocular surface,
- afferent nerve fibers,
- a central processing unit in the brain stem (that can communicate with higher brain centers) and
- afferent nerve fibers that give respective contractile stimuli to the muscles of the lid apparatus
The Brain Stem communicates with, and is influenced by, higher centers in the brain, that can regulate the lid apparatus according to what ´higher knowledge´ of superior e.g. cortical centers deems necessary. Such individual wishes of higher centers are however not always welcome to the periphery because they are one reason for rare blinking in concentrated visual tasks ... that may lead to a Dry Eye condition.
The Patho-Physiology of Disease Onset and Progression develops along the Dysfunction in the tracks of anatomy and physiology
So, by now we have a nice and more or less complete collection of tissues and functional mechanisms the are necessary to provide the OcularSurface function.
In return, when any of the involved organs or any of the trophic and regulatory mechanism is impaired, becomes dysfunctional or is completely lost ... this will also deteriorate the most basic function of the Ocular Surface which is the provision of moisture.
Therefore, Dry Eye Disease is a prototypic disease of the Ocular Surface that may always eventually occur when any of the parts of the ocular surface are altered by organ-specifc, systemic or external environmental conditions.
When Basic FUNCTIONAL COMPLEXES of the Ocular Surface are COMPROMISED ... their LACK turns into Basic CAUSATIVE FACTORS for Disease
hmmm, that sound complicated ... but it is actually very easy:
When basic functional complexes of the Ocular Surface for moisture are COMPROMISED ... this leads to a deficiency or lack:
- a LACK of Tear SECRETION - at least of one component such as
- water,
- mucin or
- lipid
- OR
- a LACK of Tear FILM FORMATION
Even a lack of only one of these two functions is sufficient to endanger the health of the Ocular Surface.
A lack of tear secretiton or a lack of tear film foRmation are Basic CAUSATIVE FACTORS for Dry Eye Disease
The lack of such basic funtions for moisture(by either secretion of film formation) - i.e. a manifest lack of moisture - is a pathologic factor for the Ocular Surface Mucosa and thus necessarily constitutes a Basic CAUSATIVE FACTORS for the onset and progression of pathology in the form of Dry Eye Disease.
For a mucosa it is a question of life or death to have the pre-requisit of being moist fulfilled ! ... this may remind us of a citation by WELLINGTON
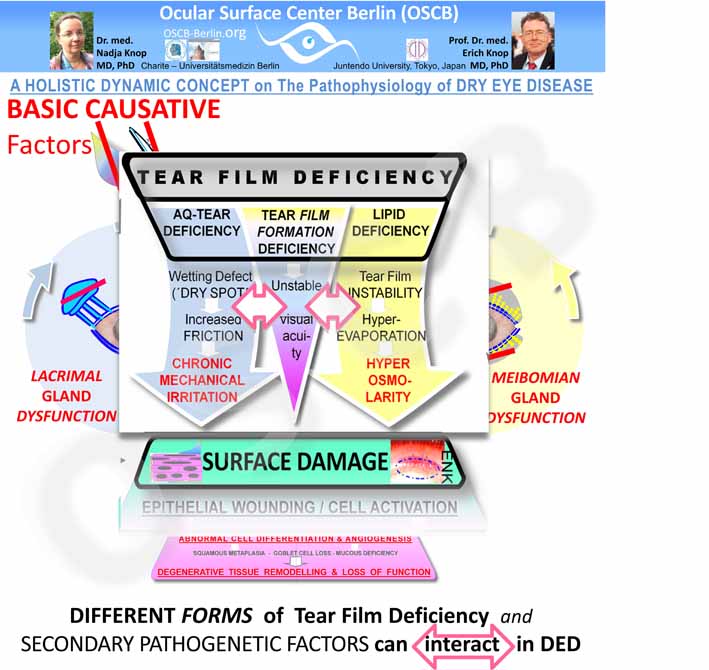
Basic causative factors CAUSE PRIMARY PATHOLOGY of the Tear Film and Ocular Surface
The basic causative factors cause the PRIMARY PATHOLOGY of the ocular surface that is already known from the early days of dry eye research:
- Tear Film Deficiency
- Surface Tissue Damage
Tear Film Deficiency is A Typical PRIMARY Pathology In Dry Eye
When a dysfunction of gland secretion of at least one component - mucins, water or lipids - of the tear film occurs this leads to Pathology of the Tear Film- termed Tear Film Deficiency. This is one PRIMARY Pathology on Dry Eye Disease.
Tear Film Deficiency typically leads to negative influences- mainly mechanical friction and hyperosmolarity - on the underlying epithelium of the ocular surface.
Tear Film Deficiency defines the type of Dry Eye Disease ... and its respective therapy
The pathology of Tear Film Deficiency is indeed so important that the different forms of Dry Eye Disease are classified/ termed according to the type of Tear Film Deficiency, as either:
- Aqueous-deficient Dry Eye or
- Lipid-deficient/ evaporative Dry Eye or ... more rarely
- Mucin-deficient Dry Eye
Surface Tissue Damage is a typical downstream alteration of tear film deficiency - BUT can also occur as a primary issue
Therefore Surface Tissue Damage is a typical downstream alteration due to a tear film deficiency of any kind and the question may arise why Surface Damage is then not designated as a ´secondary pathology´ in this concept on Dry Eye Disase.
Acutally Tissue Damage can very well arise as a first alteration of the ocular surface due to negative influences directly on the tissue, such as a nerve damage, lack of hormones or to a lack of trophic factors such as Vitamin A. Such factors that lead to a primary tissue damage are less frequent in "typical" Dry Eye Disease in the ´typical´ ophthalmological practices.
Surface Damage and Tear Film Deficiency are interdependent primary Pathologies
The interaction of the Tear Film and the Surface Tissue is more complex, as explainned in more detail in the ´Overview on Dry Eye Disease´ and is rather an interdependence that acts in both directions.
It is thus not surprising that Tear Deficiency and Surface Damage are linked via vicious circles. Tear Deficiency induces, e.g. by instability and dry spots in the tear film, downstream Epithelial Surface Damage that, in return, further reduces the binding of the tear film to the surface which then leds to more surface damage.
Since pathologenetic factors act back onto themselves and thereby amplify the disesase process this is termed a Vicious Circle.
Surface Damage and Tear Film Deficiency are so closely interrelated that it appears justified and makes most sense from a more general patho-physiological perspective on Dry Eye Disease, when Tear Film and Tissue are both designated as "Primary Pathology".
Hierarchy of Pathogenetic Factors - Causative Factors vs. Primary and Secondary Pathology
Primary Pathologies are governed by SEQUENCES of SECONDARY PATHOGENIC Factors that drive the Disease process
Basic CAUSATIVE FACTORScause PRIMARY PATHOLOGY as discussed above.
Sequences of secondary pathogenic factors thus lead to disease progression and worsening of the condition.
Secondary Pathogenetic Factors in Tear Film DeficieNCy
Sequences of Secondary Pathogenetic Factors govern the primary pathology of Tear Film Deficiency - and interact with each other. The secondary pathology terminates in Chronic Mechanical Irritation by Friction and Hyper-Osmolarity as the main factors that induce Damage of the Surface Tissue.
Tear Film Deficiency gives rise a sequence of various Secondary Pathogenetic Factors. Examples are known to most clinicians and encompass factors such as:
- Instability of the tear film with early Break-Up
- formation of Dry Spots at the Ocular Surface
- increased friction
- chronic mechanical irritation
- hyper-evaporation
- hyper-osmolarity of the tear film
The Different Types of Tear Film Deficiency that determine the Type of Dry Eye Disease tend to mix with increasing severity of disease. This is conceivably due to the impairment of more and more functional complexes with downstream negative effects as the disease process proceeds, destroys for tissues and becomes more severe.
It is difficult to allocate such secondary pathology to specific types of tear film deficiency.
Lipid deficieny is e.g. typically discussed together with tear film instabilty which is then though to be linkes to hyper-evaporation of the aqueous phase a reason hyper-osmolarity of the the tear film.
On the other hand, wetting defects are often discussed in the context of the formation of dry spots as regions where increased friction due to decreased lubrication occurs which eventually leads to chronic mechanical irritation.
In fact, the factors in secondary pathology are interacting which is indicated in the diagramm.
There is some indication to think that different types of Dry Eye Disease may only be clearly discernable in initial phases of the development and progresssion of the typically chronic disease process ... and tend to mix progressively as the disease progresses and affects more functional circuits with accumulatinng pathology.
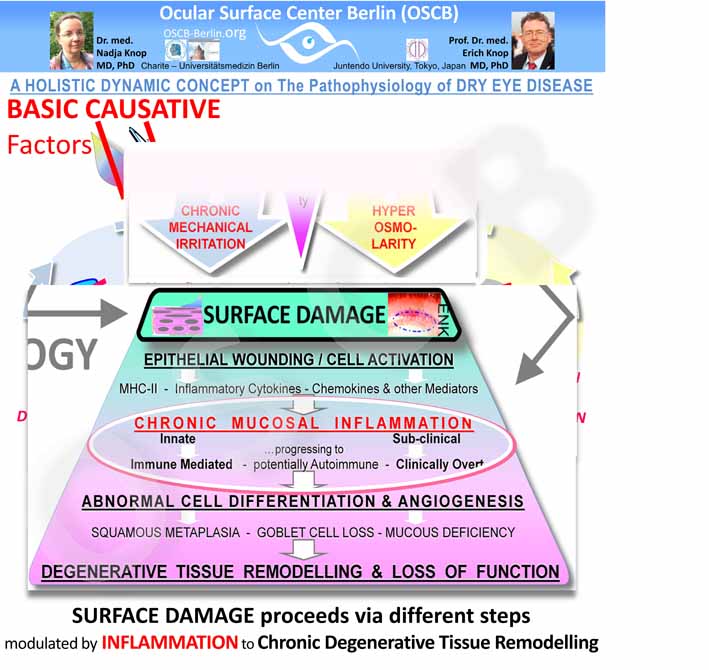
Secondary Pathogenetic Factors in Ocular Surface TISSUE DAMAGE reflect aspects of Inflammatory Cascades
Secondary Pathogenetic Factors in SURFACE Tissue DAMAGE also form Sequences of increasing severity that propagate the disease process. Chronic inflammation is the main amplifier of disease - it gives rise to several Vicious Circles and to a Chronic Tissue Remodeling with Loss of Function.
The secondary pathogenetic events that occur in SURFACE TISSUE DAMAGE reveal characteristics of pathways of chronic mucosal inflammation.
Apparently the primary impact is on the epithelial cells of the cornea and conjunctiva which is in line with the observation that typically an insult typically comes from the outside, i.e. the luminal region, i.e. here the tear film - even though pathology can also start in the tissue, as discussed above.
Chronic alteration of epithelial cells at the Ocular Surface induces a Chronic Inflammatory Process
Inflammation as such is no major problem in principle because it is a very basic protective answer of tissues to many noxious stimuli that intends to remove the negative stimulus. Inflammation is a regulated process and thereby limited and typically ends with a repair reaction.
A schematic mechanistic diagram shows some KEY EVENTS in Mucosal Inflammation during Dry Eye Disease
Inflammatory processes are typically first innate and subclinical - which means is does not or very limited show the typical clinical signes of inflammation. The absence of redness, swelling, heat and pain. Therefore the impression that such signs are absent in patients does not tell there is no inflammation.
Chronic inflammation progresses to an immune-modulated inflammation
Inflammation becomes problematic
- when it becomes chronic - and therefore unlimited - and
- when an innate inflammation involves the specific immune to turn into an immune-mediated inflammation - which can strongly amplify the inflammatory process and
- when a transformation of the immune-mediated inflammation into an auto-immune disease may occur
At the ocular Surface in Dry Eye Disease unluckily but typically two of these problems exist - chronicity and immune-modulation. Auto-immune disease in Dry Eye is presently only shown in a mouse model but may also be possible in the human.
This includes:
- the chronicity of the tissue irritation when the deficiency of the tear film persists or even becomes worse due to the interdependency of the integrity of tissue and tear film, as discussed above
- the wounding and activation of cells with a build-up of an inflammatory micro-milieu - eventual destruction of cells. Downstream events are:
- upregulation of adhesion molecules on vascular endothelial cells & recruitment of lymphoid cells from the vascular compartment
- upregulation of antigen-presentation molecules and co-stimulatory molecules
- aberrant antigen-presentation due to the continuous presence of of inflammatory danger signals that can deregulate antigen-presentation
- presentation of auto-antigens from own cells to lymphoid cells in the context of inflammatory danger signals that can lead to auto-immunity.
- activation of proteases (Matrix-Metalloproteinases, MMPs) that degrade the connective tissue stroma
Chronic Inflammation results in downstream secondary pathogenetic factors such as:
- abnormal cell differentiation with squamous metaplasia,
- loss of goblet cells and their mucins
- thus a loss of surface wettability
- leading to increased tear film instability
- neovascularization with formation of new blood and lymph vessels that
- destroy the corneal transparency
- drive the recruitment of more lymphoid cells and other leukocytes
- drives the inflammation
- impairment of normal cell differentiation that contributes e.g. to squamous metaplasia and loss of mucins
- chronic cycles of inflammatory destruction of the connective tissue to provide space of an effective inflammation that run in parallel with frustrane repair mechanism with formation of scar tissue - this leads to Degenerative Tissue Remodeling
Chronic inflammation is an important factor for amplification of the disease process in Dry Eye
In a worst case scenario, such chronic ocular surface inflammation can lead to Degenerative Tissue Remodeling with Loss of Function as shown in the mechanistic diagram.
VICIOUS CIRCLES in Dry Eye Disease
VICIOUS CIRCLES are actions of pathogenetic negative factors that eventually act BACK onto themselves.
VICIOUS CIRCLES are not new in Dry Eye Disease and Members of the Ocular Surface Center Berlin (OSCB) have frequently suggested Vicious Circles in Concepts for Dry Eye Disease in various publications (see the little collection dating back to the year 2000 above).
Pathogenetic amplification loops termed Vicious Circles often have interposed further factors before they act back. Vicious circles are thus not always immediately detectable.
EFFECT of VICIOUS CIRCLES
=> By vicious circles a pathological process is amplified and progresses, gets worse and tends to perpetuate if it is not interrupted by suitable and timely therapeutic intervention.
It is an aim of this homepage to spread the knowledge of ocular surface disease and its important disease mechanisms in order to promote a timely diagnosis and therapy.
Vicious Circles are often over-simplified
When people had adopted the idea of Vicious Circles in Dry Eye Disease, as e.g. in the DEWS Workshop Report 2007, the concept was put in an over-simplified and thus misleading way as a one large single Vicious Circle.
However, a single vicious circle is misleading - it is half true and half wrong ... such ideas usually cause most problems.
- it is right that Dry Eye Disease indeed has amplification mechanisms that perpetuate the disease process.
- but it is wrong and misleading that this is one single vicious circle - because this implies the misleading suggestion that therapy can interfere anywhere in this proposed circle ... and will still always successfully interrupt the disease process in Dry Eye.
The latter is obviously wrong ... as the experience in patients with Dry Eye Disease has shown over the years !
Vicious circles in Dry Eye Disease must be carefully identified in the individual patient - in order to find an effective therapy
When we think for example of Lipid Deficiency due to Meibomian Gland Dysfunction, that turned out to be the most frequent type of Dry Eye Disease it becomes obvious, that it actually does matter whether
- these patients use aqueous tear substitution which will conceivably quickly evaporate together with the own aqueous tears - because the evaporation limiting lipids are missing
- OR
- whether it is substituted what is missing - which is lipids in this case- and thereby apply a patho-physiologically adequate therapy option that will conceivably be more effective
several, Different, interacting, Vicious Circles OCCUR in Dry Eye Disease - that were hitherto not recognized,
Members of the Ocular Surface Center Berlin (OSCB) have identified several different and interacting Vicious Circles in Dry Eye Disease - not just one as frequently assumed.
Vicious Circles do not necessarily depend on inflammation, even though inflammation, as a mighty cell biological process, gives rise to many of them.
Members of the Ocular Surface Center Berlin (OSCB) could identify several different interacting vicious circles in tissue and tears during Dry Eye Disease.
Vicious Circles "drive" the disease process - they are ´Patho-Physiology in a move´ and represent the dynamics that the practical clinical course of Dry Eye Disease has.
In order to make these DYNAMICS IN DISEASE understandable - DYNAMIC VISUALIZATION tools such as the ANIMATIONS used here on the Internet pages of the Ocular Surface Center Berlin (OSCB) are superior in many aspects to ordinary static representations and diagrams.
Exact Identification of the different Vicious Circles and their interaction in the individual patient is essential for an effective therapy
It is important to be aware of the different Vicious Circles and their interactions in order to understand Dry Eye Disease and its progression sufficiently.
Understanding of the vicious circles that are active in an individual patient is important for an effective therapy - which is a notorious cardinal problem in Dry Eye Disease as we know !
One important Vicious Circle links the two Primary Pathologies of Tear Deficiency and Surface Damage
A vicious circle that does not primarily depend on inflammation closely links an interrelates Tear Film Deficiency and Ocular Surface Damage.
This makesthe two primary pathologies closely interrelated and is based on the facts that:
- TEAR FILM DEFICIENCY induces Surface Damage through Chronic Mechanical Friction and Hyper-osmolarity
- ... and in return ...
- SURFACE DAMAGE reinforces Tear Film Deficiency -
- because dry spots on the surface with loss of microvilli and mucus further deteriorates the wettability of the epithelial cell surface and thus the tear film stability
- ... and so on ...
The Dysfunction of the Ocular GLANDS that occurs in Dry Eye Disease proceeds in PATHOLOGICAL CAROUSELS ... which are Vicious Circles
The Surface Tissue Damage that occurs in Dry Eye Disease and proceeds via a sequence of secondary pathogenic factors - with chronic mucosal inflammation as a major amplifying factor - also involves the tissue of the ocular GLANDS.
The ocular GLANDS are an integral part of the ocular surface, like the main and accessory lacrimal glands and the Goblet cells of the conjunctiva. The Meibomian glands are only separated from the conjunctival sac by the conjunctival tissue itself - for details, please see the section ´Ocular Surface´.
Inflammation-dependent Vicious Circles in the Tissue booster SURFACE Damage and Progression to chronic inflammation
There are at least two clearly inflammation dependent vicious circles that occur during the pathology of Surface TISSUE DAMAGE.
Both of these Vicious Circles originate from the abnormal cell differentiation in the tissue with angiogenesis and driven by the chronic inflammation that gives rise to the corrupted tissue differentiation. Squamous metaplasia with loss of goblet cells and mucins is also, at least in part, promoted by inflammatory mediators.
The abnormal tissue cell and tissue differentiation acts in 2 Vicious Circles
- one acts back up and prevents the reparative reformation of normal morphology of the of the surface epithelium during dry eye disease
- the other directly feeds back to amplify inflammation, because chronic inflammation, with all its downstream pathways,
- recruits large amounts of leukocytes and lymphocytes into the tissue from the vascular compartment and
- corrupts the antigen presentation
- thereby further deregulates the normal physiologic immune tolerance
- which leads to further damage
Chronic Mucosal Inflammation of the Ocular Surface includes the Ocular Gland Tissue
Inflammatory events play a role in the Dysfunction of both main Ocular Glands - the Lacrimal Gland and the Meibomian Glands.
Lacrimal Gland Dysfunction (LGD) is the most prominent cause for Dry Eye Disease but, as now widely known, it is not the most frequent cause. Sjögren´s Syndrome, the main reason for primary LGD, is an auto-immune inflammation of this mucosa-associated gland. The more frequent sensory nerve impairment occurs mainly due to inflammatory events at the ocular surface.
Meibomian Gland Dysfunction (MGD) is also promoted by inflammatory events of different kinds that integrate MGD into the Vicious Circles - ´Pathological Carousel´ of Gland Destruction - please see below.
A major concept for understanding of aqueous Tear deficiency is sensory nerve impairment due to InflAmmation
A major concept for aqueous tear deficiency in Dry Eye Disease is an afferent sensory nerve fiber impairment due to chronic inflammatory processes at the bulbar surface (cornea and conjunctiva) in dry eye disease. Dysfunction of the afferent sensory nerves will lead to a dysfunction of the neural reflex arc for driving the efferent innervation for secretion of the lacrimal gland.
A major concept for understanding of the ´typical´ ´ordinary´ aqueous tear deficiency due to LGD in Dry Eye Disease is
- an afferent sensory nerve fiber impairment
- that is thought to occur due to ongoing inflammatory processes at the bulbar surface (cornea and conjunctiva)
- that leads to impairment of the neural reflex arc (via the cranial nerves V and VII) for driving the secretion of the lacrimal gland
- and will thus lead to dysfunction of the dependent efferent secreto-motor innervation to the lacrimal gland
as explained in two seminal papers by Mike Stern, Steven Pflugfelder and colleagues
The underlying reason for such ocular surface inflammation may be:
- either due to a primary disease of the Lacrimal gland such as Sjögren´s Syndrome or to viral infection such as e.g. by Epstein-Bar Virus
- or secondary due to any other condition that may lead to onset of an inflammatory chronic Dry Eye Disease. This can occur secondary to MGD, to systemic disease, to impairment of regulatory systems and to environmental risk factors - as explained in the ´Overview on Dry Eye Disease´.
Meibomian Gland Dysfunction (MGD) depends at least in part on inflammatory events
In Meibomian Gland Dysfunction (MGD) at least parts of the pathology also depend on inflammatory events.
Inflammatory events in MGD, at some difference to the lacrimal gland, seem to be mainly subclinical
- which is supported by the observation in the available histological investigations that lymphoid cells do typically not occur.
- Some evidence from confocal investigations, which however have a very limited resolution in this respect, seem to indicate that inflammatory cells may sometimes be involved in the pathology.
An important concept for the understanding of MEIBOMIAN GLAND DYSFUNCTION is Obstruction
An important concept for the understanding of MEIBOMIAN GLAND DYSFUNCTION is Obstruction of the terminal duct and orifice of the Meibomian Gland due to mainly 2 factors:
- INCREASED VISCOSITY of the Meibomian lipid secretum
- conceivably due to the influence of metabolic products such as lipolytic enzymes
- produced by an increased colonization with the normal commensal bacterial species
- together with
- INCREASED EPITHELIAL KERATINIZATION (termed hyper-keratinization) due to
- irritant lipid species or bacterial products or
- soluble inflammatory mediators produce in the gland during sub-clinical inflammation
- the influences of age
- a lack of sufficient androgen sex hormone levels
- or potential other factors
Meibomian Gland Dysfunction (MGD) seems to be negatively influenced
- by chronic mechanical irritation in contact lens wear because long-term contact lens wear leads to a distinct reduction of the gland tissue by disappearance (drop-out).
- by chronic inflammatory Ocular Allergy which is largely affecting the tarsal conjunctiva where the Meibomian glands are located. This has a similar negative effect on the glands.
as observed by Arita and colleagues
- I may therefore be concluded that
- mechanical and inflammatory stimuli both reach the Meibomian Glands, either by direct translation of mechanic friction to the glands, or by the diffusion of soluble inflammatory mediators through the conjunctiva
- since chronic mechanical irritation can lead, via activation of the the epithelial cells, to production of inflammatory mediators the stimulus on the Meibomian glands may in both cases be due to the diffusion of soluble inflammatory mediators
The progression of Dry Eye is Promoted by Gland Dysregulation - driven by Vicious Circles that form PATHOLOGICAL CAROUSSELS
Pathological Carousels of Gland Dysregulation link the pathology in the glands and at the "surface" of cornea and conjunctiva in a mighty Vicious Circle.
It is evident, that the progression of pathology in the glands affects and drives the disease process in Dry Eye Disease - on the other hand inflammation of the conjunctival surface will impair the innervation and thus promote Gland Dysregulation. This constitutes a Vicious Circle
- It must be assumed, that a progression of pathology by the described sequences of secondary pathogenetic factors, i.e. cell activation, inflammation, progressive tissue destruction and loss of function, also applies to the ocular gland tissue and propagates the disease process inside the glands
- the progression and worsening of disease in the glands would certainly negatively influence the function of the ocular surface which mainly serves, as described above, for the maintenance of moisture - and thus a LACK of Secretion was identified as one of the two basic causative factors for Dry Eye Disease.
- it must therefore be concluded that the described interaction between the "surface´, of conjunctiva and cornea, and the associated glands acts BACK in a Vicious Circle that reinforces the disease process in both of them.
The Vicious Circles of Gland Destruction are termed as a PATHOLOGICAL CAROUSELS of Gland Destruction by members of the Ocular Surface Center Berlin. This appears to represent an important new factor in Dry Eye Disease.
tissue pathology OF the eye ball can induce pathology of the Eye LID
Pathology of the Surface TISSUE that feeds into Pathological CAROUSELS of GLAND DYSFUNCTION can further promote Pathology of the Eye LID.
Clinical Observation:
Patients with pathological conditions of the ocular surface that go along with increased mechanical friction - Dry Eye Disease and Contact Lens wear - have a high prevalence of a pathological vital stainable alteration of the epithelium of the Lid Wiper zone at the posterior lid border. This was termed LID WIPER EPITHELIOPATHY (LWE)
and described by Donald Korb and colleagues
- for more detailed information please see the section on the ´Lid Wiper´.
Histological Observation:
Members of the Ocular Surface Center Berlin (OSCB) could show by histological examination that frequent pathological cells occur at the epithelial surface in Lid Wiper Epitheliopathy (LEW) and in such zones were less Goblet cells than typical for the Lid Wiper and necessary there as a buit-in lubrication system.
Pathology of the Lid Wiper is linked via a Vicious Circle to pathology of the bulbar surface ... and reverse
It must therefore be assumed that patients with epithelial lid border defects in LWE and consequent reduced lubrication
- will have decreased adherence of the aqueous tear film and
- this will exert an increased friction on the epithelium of the cornea and conjunctiva over which it travels more than accumulated 100 meters a day
- this will induce or amplify mechanical alteration of the bulbar epithelium
The described interaction of Bulbar Surface and Lid Wiper constitutes another VICIOUS CIRCLE
- tissue pathology at the eye ball is
- translated into the ocular glands
- by the above described pathological carousels of gland dysfunction and
- eventually is translated into lid wiper epithelium of the posterior lid border
- from where is acts BACK, as characteristic for vicious circles, onto the eye ball
Write here...