OVERVIEW ...
... on the Function of The OCULAR SURFACE & some Details on DRY EYE DISEASE
Choose your CHAPTER of Interest - or simply read along ... which may be most instructive
BASIC FUNCTION
of the Ocular Surface
The Ocular Surface is a permanently MOIST TISSUE
The OCULAR SURFACE is the moist tissue at the anterior side of the eye ball
Moisture is necessary to preserve its health and integrity - and it is thus a pre-requisite for VISION.
MOISTURE comes from the Tears and is produced by the Ocular Glands - but it must be spread into a Tear FILM by the BLINK Movement of the Eye Lids ... to make moisture PERMANENT - Everytime and Everywhere !
Basic Functional Complexes
The Glands of the Ocular Surface produce the Tears.
The Tears are the essential medium for the provision of moisture at the Ocular Surface.
The Eye Lids spread the tears into the essential pre-ocular Tear Film.
The Tear Film makes it possible that moisture can even persist on the tissue within the opened palpebral fissure - and the Tear Film aids in allowing a perfect light refraction and thus a perfect vision at the same time.
The Healthy Ocular Surface is a Pre-Requisite for Vision and without it all later steps of the vision process are meaningless.
CAUSATIVE FACTORS
for Dry Eye Disease
DRY EYE DISEASE is a ´dog of many names´
DRY EYE DISEASE is medically also addressed as ´Keratoconjunctivitis Sicca´ - which means ´dry inflammation of the cornea and conjunctiva´ or only as the ´Sicca Syndrome´ (bunch of symptoms related to dryness) . This condition has various colloquial names such as simply ´dry´ eyes, ´ocular dryness´, ´itchy eyes´´heavy lids´ or ´tired eyes´ etc.
The Disease MECHANISM is relatively simple and therefore this condition is relatively frequent
DRY EYE DISEASE IS AN ALTERATION OF THE TEAR FILM AND TISSUE
Dry Eye Disease typically shows the two PATHOLOGIES of
- Tear FILM Deficiency with an unstable tear film that shows e.g. early break-up, increased evaporation, low tear meniscus.
- DAMAGE of the ocular surface tissue is the other basic pathology in Dry Eye Disease. It typically results from Tear Film Deficiency of any kind. A deficient, unstable tear film layer can no longer protect the surface tissue. Therefore the very susceptible surface cells will then immediately start to develop drying alterations that damage the tissue.
- Rarely does Surface Damage occur as a first pathology due to a different pathology such as, e.g. in a severe malnutrition with Vitamin A or due to inflammatory local or systemic disease conditions. In less developed regions of the world, however, pathologies such as malnutrition and inflammatory disease can be more frequent. A Dry Eye can thus occur more often due to a primary Tissue Damage which then deteriorates the Tear Film.
THE BASIC CAUSATIVE FACTORS FOR DRY EYE DISEASE ARE A LACK OF TEAR SECRETION AND OF FILM FORMATION
The basic CAUSATIVE FACTORS for Dry Eye Disease are those that directly lead to the deficiency of the Tear FILM - this is
- a quantitative or qualitative LACK/ Deficiency of TEAR secretion by the Glands
- and/ or
- any LACK/ Deficiency of Tear FILM FORMATION that occurs by negative influences on the BLINK MECHANISM of the EyeLids that distribute the Tears into the pre-corneal Tear Film
MAIN SIGNS & SYMPTOMS
CLINICAL SIGNS
of Dry Eye Disease
The main clinical signs of Dry Eye Disease are thus:
INSTABILITY of the pre-corneal Tear FILM:
Instability of the Tear Film is a typical feature of any type of Dry Eye Disease and thus important to be investigated.
- the normal tear film should be stable for at least 10 seconds before a rupture or "break-up" occurs
- this parameter is termed "Tear Film Break-Up Time", typically abbreviated as "BUT"
- it is typically and easiest determined by applying the vital stain fluorescein into the tears.
- The use of fluorescein solution in the test is termed as FBUT. It may already change the tear film to a certain extent ... but if the amount of additional volume is limited and when the procedure is always performed identical the FBUT Test will lead to consistent and meaningful results
- The FBUT Test has therefore been used for decades with great success.
- Meanwhile non-invasive methods (NIBUT) are gaining increased interest where the tear film break-up is detected by changes in its reflection, which is slightly more accurate in principle but requires specific technical equipment.
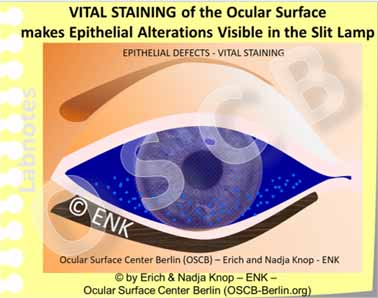
Vital STAINING of the Ocular Surface Epithelium:
Vital staining is a quick and easy way to verify another important feature of any type of Dry Eye Disease which is alteration, wounding and destruction of the normal epithelial structure
- When the tear film breaks up
- the lubrication between the bulbar surface, including a possible contact lens, and the eyelids is reduced
- this leads to increased friction and thus to increased mechanical damage of the surface cells
- it exposes the underlying ocular surface epithelium to the air atmosphere
- in addition a local thinning of the tear film by evaporation is shown to result in spots of increased osmolarity of the remaining tear fluid and thus in hyper-osmolarity
- this leads to chemical damage of the surface cells
- The air exposure and the mechanical and chemical damage of the surface epithelium results in pathological alterations of the ocular surface with cell destruction
- cell destruction can be marked by stains that are applied in clinics to the living eye - the stains are therefore termed vital stains
- vital stains bind to the altered surface and thus result in little stained spots where damage has occured.
- Ocular surface damage is a typical characteristic of ocular surface disease and in particular of Dry Eye Disease. The degree of vital staining therefore shows the degree of ocular surface damage.
- Surface staining in the temporal part is the inter-palpebral zone is thought to be more characteristic for Dry Eye Disease than a more nasal staining.
Typical SYMPTOMS
The pathology of Dry Eye Disease gives rise to some typical subjective SYMPTOMS
Tear Film Deficiency and Surface Damage lead to typical subjective irritative SYMPTOMS of the patient.
Typical Syptoms in Dry Eye Disease are e.g. ocular irritation, dryness and grittiness, often described as ´heavy eye lids´ or ´tired eyes´, together with an unstable visual acuity and episodes of blurred vision, with various degrees of irritation and pain.
Initially the ocular irritation due to tissue alterations can lead to episodes of increased tearing, watery eyes and tear dripping over the lid margin.
Frequent RISK FACTORS
for DRY EYE DISEASE ... and their Self-Perpetuating INTERACTION
A certain Challenge in the understanding of Dry Eye Disease is based on the fact, that it can be initiated and influenced by a large variety of different factors
The ONSET and PROGRESSION of Dry Eye Disease is strongly influenced by many different factors.
- REGULATORY SYSTEMS of the body such as the nerve system, the endocrine hormonal system and the immune system have great importance.
- There are additional RISK FACTORS, that have a negative influence on the tear fluid or on the ocular surface tissue and thus increase the likeliness for the onset and progression of disease.
Unluckily, Dry Eye Disease has a certain inherent tendency to self-enforce and perpetuate itself, if not timely diagnosis and effective therapy is performed
The two typical pathologies
in Dry Eye Disease are
- Tear FILM DEFICIENCY and
- Surface TISSUE DAMAGE
Tear Film Deficiency and Surface Damage influence each other negatively and are therefore linked by self-enforcing vicious circles that lead to worsening of the condition.
Inflammatory Reactions
are a typical component of Dry Eye Disease because they represent basic protective mechanisms of wounded tissues, as also occurs at the Ocular Surface.
When the wounding becomes chronic the inflammatory answers of the tissue also become chronic and more severe.
Inflammatory pathways are thus an important disease mechanism for worsening of the condition in chronic ocular surface disease.
An occasional ´Dry´ Eye condition can certainly happen also in healthy individuals under certain conditions - however, when this becomes chronic, it can develop into a disease
Occasional ocular DRYNESS can certainly occur once in a while also in healthy individuals. Such dryness typically depends on adverse environmental factors, is short-lived and disappears quickly after some vigorous eye blinks or when the negative factors are removed. When the condition becomes chronic, however, an occasional ocular dryness can turn into a manifest permanent Dry Eye DISEASE.
CONTACT LENSES and the Ocular Surface
CONTACT LENSES are a fantastic Optical Tool - with pros and cons
Contact Lenses are a fantastic Optical Tool that has long been desired by many individuals with refractive disorders.
They became eventually widely usable only in the second half of the 20th century and have seen great.improvements since then.
CONTACT LENSES correct refraction directly on the Cornea ... with clear optical advantages
´Rigid´ Contact Lenses are typically smaller and exclusively rest on the cornea. They need a certain adaptation time for the wearer and are thus less widespread, but have superior inert material and optical quality.
Contact Lenses can correct refractive errors directly on the cornea and therefore, they have some principal optical advantages compared to spectacles.
Contact Lenses certainly provide greater ´freedom´ for the user in a lot of sporting, outdoor and society activities.
There are different basic types of Contact Lenses. Soft hydrogel Contact Lenses are the most widely used type.
Soft lenses can typically be worn without distinct irritation and thus often require no adaptation time for the wearer to get used to a lens.
This may be a reason why most Contact Lenses are of the ´Soft´ type and are not worn for medical but for esthetic/ cosmetic reasons.
CONTACT LENSES are swimming in the Tear Film and have influence on its stability and evaporation rate
Movement of a Soft Contact Lens on the Surface of the Eyeball and behind the Eyelids. The Contact Lens moves with every gaze movement of the eyeball and also upon the frequent eye blinks. The amount of mechanical friction at the ocular surface is typically increased in contact lens wear, even when the tear film is sufficient.
The fact that Contact Lenses are sitting in the middle of the Ocular Surface has some pros and cons.
They certainly have some clear optical advantages ...
... but contact lenses still represent a ´foreign body´ for the Ocular Surface Tissues and Tear Film.
Even though contact lenses are typically ´swimming´ in the tear film it is still inevitable, that they are in mechanical contact with the ocular surface tissues.
A typical side effect of contact lenses therefore is the occurrence of increased frictional forces to the ocular surface tissues.
CONTACT LENSES can have negative influence on the Ocular Surface Fine Structure
The fine structure of the surface epithelium may undergo a deterioration where it is exposed to the influence of a Contact Lens. Shown here is the change of the bulbar conjunctival epithelium in the excursion zone of a soft Contact Lens. The cubical surface cells with interspersed goblet cells for the production of water-adhesive mucins are replaced by a squamous epithelium without goblet cells in a process termed ´squamous metaplasia´.
Although fitting principles usually try to avoid too much physical ´touch´, contact lenses are still, inevitably, in contact with the ocular surface - just as their name suggests.
Contact lenses can thus have mechanical, physicochemical and chemical impacts on the Ocular Surface to varying degrees
This concerns particularly the interference of the contact lens with the very sensitive central cornea and the similarly sensitive posterior lid border.
The conjunctival areas on the eyeball and on the back side of the lids are less sensitive, but are also in touch with the contact lens and are thus exposed to potential negative influences.
It is known for decades that chronic friction by a contact lens may negatively influence e.g. the fine structure of the conjunctival surface and thus reduce the wettability of the ocular surface. A typical side-effect in long-term contact lens wear is the potential development of Dry Eye symptoms of varying degrees.
Ir is shown that the structure of the bulbar conjunctiva changes in contact lens wear. This occurs in the zone where the margin of the contact lens is in touch with the surface and rubs over it upon every movement of the eye. The type of epithelium changes, termed as squamous metaplasia, and the number of goblet cells that produce the important mucus for the wetting of the surface, decrease in number. These alterations deteriorate the wetting of the Ocular Surface and promote the onset or worsening of Dry Eye Disease.
The Fitting of a Contact Lens determines its impact on the Ocular Surface:
- in flat fitting the Contact Lens exerts a certain pressure particularly on the center of the cornea
- in steep fitting the margin of a Contact Lens is rubbing particularly on the bulbar conjunctiva
- in every type of fitting a mechanical interaction of the Contact Lens margin with the very sensitive posterior lid border is inevitable due to the blink movement of the upper eyelid
Speciality Contact Lenses can serve as a medical tool
Apart from the fact that Contact Lenses can exert unwanted side effects on the ocular surface and tears Contact Lenses can also be used as a medical tool in selected cases.
The easiest case is probably when a soft Contact Lens is used as a clinical bandage lens to promote healing after surgery or in cases of recurrent corneal defects (erosions)
Several types of Speciality Contact Lenses exist that can be used as medical tools in selected medical conditions for patients who are in continuous clinical control.
This refers to ´Rigid´ Contact Lenses that can correct higher degrees of corneal shape distortion (as occurs in higher astigmatism and in keratoconus) where the visual acuity can not be sufficiently corrected by spectacles.
´Rigid´ Contact lenses can also be used for intended changes of the corneal shape, termed as ´Orthokeratology´ in order to avoid day time wear of spectacles - which certainly needs close clinical monitoring.
SCLERAL Contact Lenses
Even though contact lenses lead to alterations of the ocular surface fine structure with occurrence of dry eye symptoms ...
... Speciality Contact Lenses (Scleral Lenses) can be used as a medical tool in patients with severe Dry Eye Disease.
Scleral Contact Lenses provide a protecting translucent cover over the sensitive cornea and constitute a moist chamber that preserves the patient´s few own tears under the vault of the contact lens against evaporation. This can typically restore ocular surface healing and visual acuity.
HYGIENE is still a CRUCIAL FACTOR in Contact Lens Wear in order to avoid infections
Modern contact lens types can often reduce many of the potential negative impacts on the ocular surface by technical improvements - An issue that is still relevant is, however, the HYGIENE.
Insufficient Hygiene is a crucial factor in Contact Lens wear and results in a higher rate of ocular infections in contact lens wearers. Microbes can be introduced by the fingers of the wearer or from the use of tap water, that should be omitted. Certain types microbes also occur on the normal ocular surface. Microbes grow on the lenses and in the storage containers and form adhesive ´biofilms´ that protect them against cleaning and removal.
When basic rules of hygienic contact lens wear are not respected this can still result in dangerous ocular infections that may endanger vision.
Even with application of the most advanced medical therapy, a severe contact lens related corneal infection may eventually and tragically lead to a loss of the eye.
Bacteria are typically introduced through the handling of the contact lens by the wearer and/or by use of contaminated tap water. Bacteria accumulate in the contact lens containers or in difficult to remove deposits on the contact lens itself.
The occurrence of infection is further promoted by the inevitable occurrence of tissue microtrauma of different kind in contact lens wear. This provides a route of entry through the normally almost impenetrable ocular surface barrier.
Particularly inexperienced Contact Lens wearers are at risk for serious ocular infections. Furthermore patient groups with a reduced level of immune defense such as children and elderly people are particularly susceptible to ocular surface infections.
The increased use of daily disposable contact lenses contributes to a decrease in ocular infections. because the critical steps of cleaning and storage of a worn lens become obsolete.